Integrated Healthcare for Children: The Child Health Hub
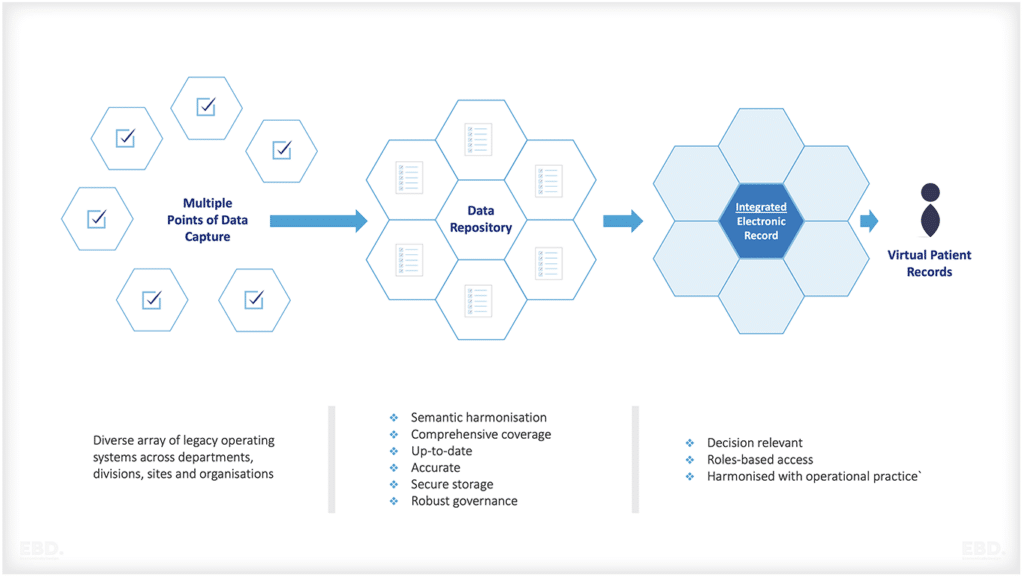
An “ideal” child health system can be described as one that acknowledges the distinct requirements of children, young individuals, and their families. It guarantees access to exceptional paediatric expertise and enables the smooth integration of timely information, effective communication, accurate data, and comprehensive care.
The Child Health Hub (CHH) is a pioneering example of integrated healthcare specifically designed for children, young individuals, and their families.
In this economic lens we explore why integrated healthcare is important for children, The Child Health Hub model and how it has been applied in north west London. We also examine models of integrated healthcare for children from other countries.
The Child Health Hub is designed to overcome the traditional challenges that can arise within healthcare systems, such as fragmented care delivery and uncoordinated patient management. It also aims to deliver a collaborative health model between paediatricians, general practitioners, allied health professionals, and other public services in the service users’ local communities.
Why is integrated healthcare for children important?
Integrated healthcare for children prioritises their unique needs by establishing a comprehensive and interconnected network of tailored medical care. This approach enhances continuity and effectiveness through seamless information sharing among multiple providers.
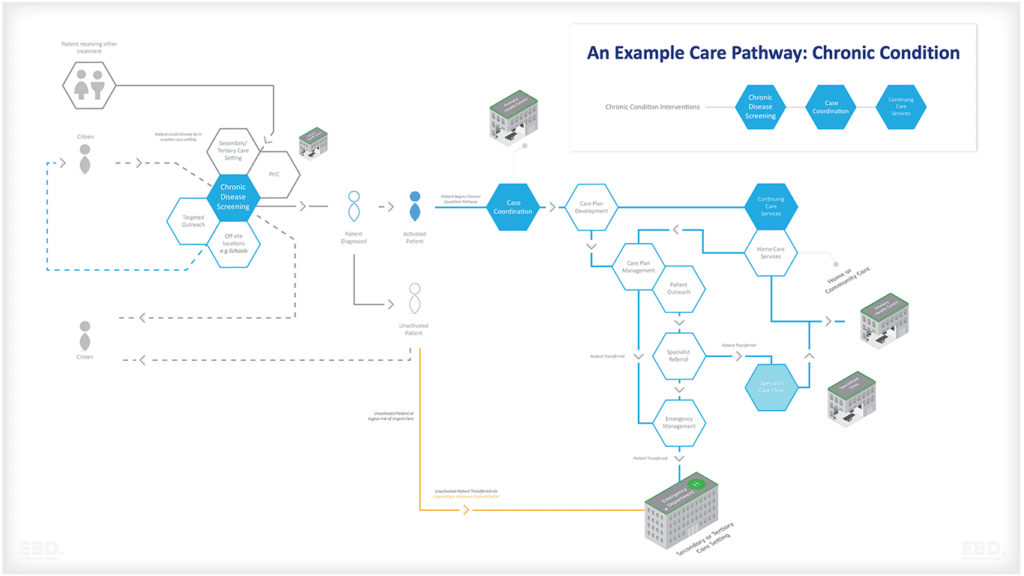
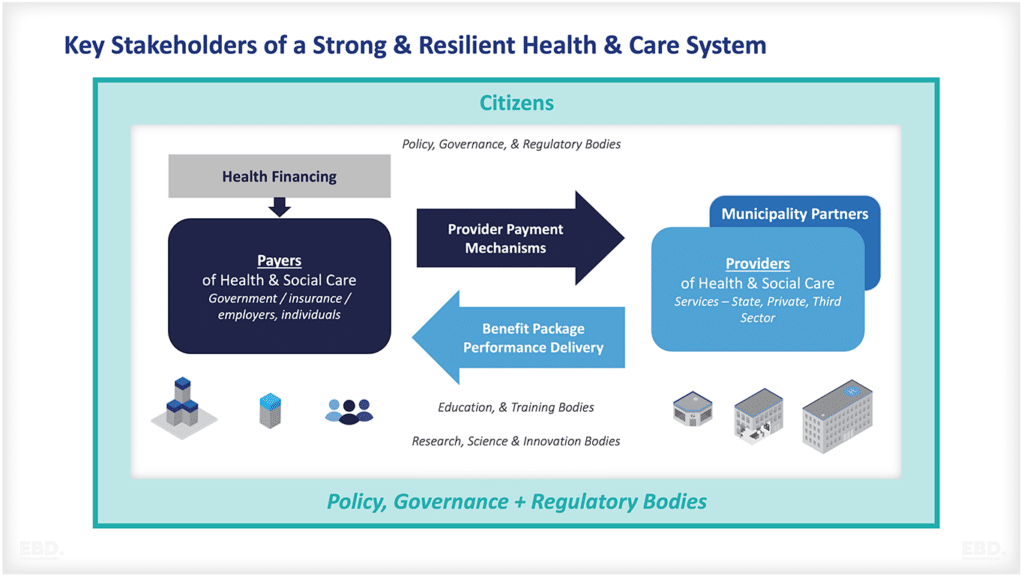
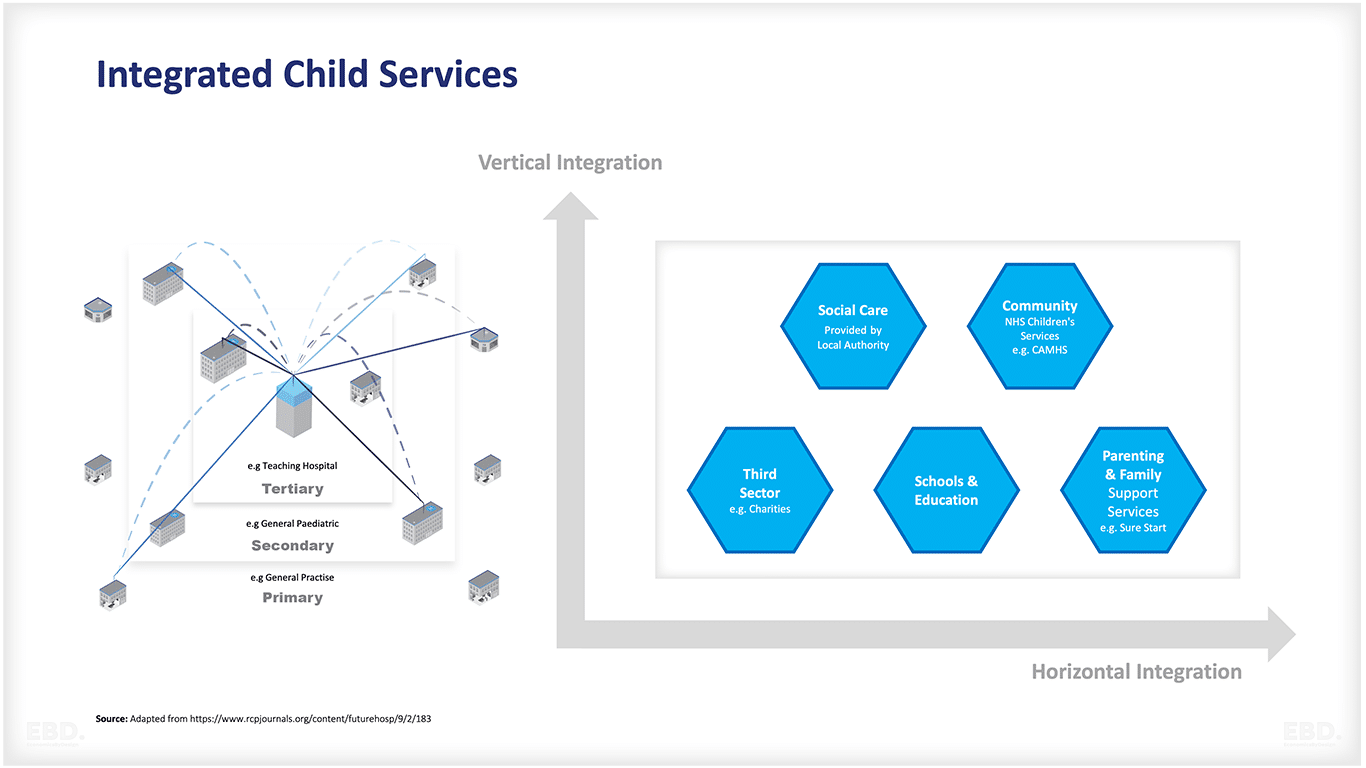
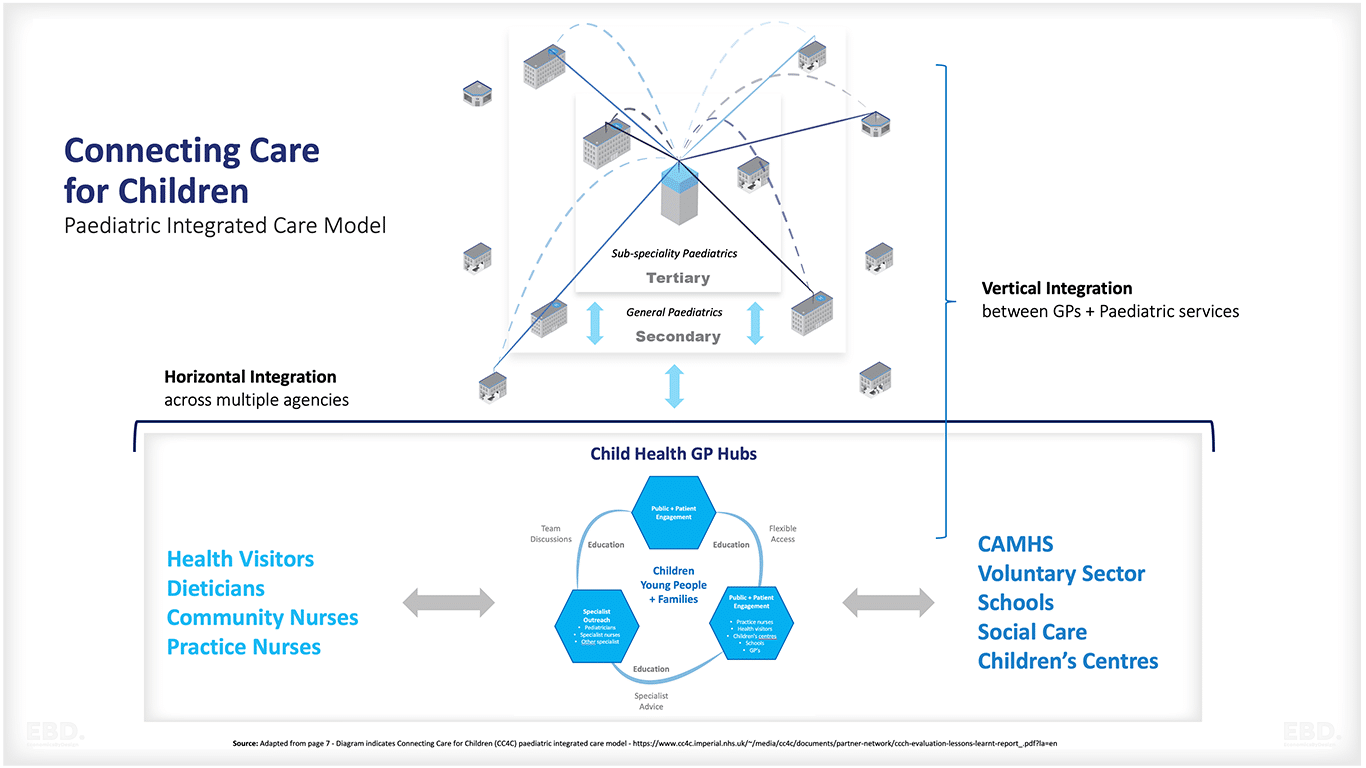
Vertical integration occurs when providers collaborate across different levels, while horizontal integration involves collaboration among different sector providers at the same level. Both types of integration aim to deliver holistic care.
Current challenges in NHS health and care services for children and young people
Currently, there exist several challenges and issues concerning the child health service. These issues can have significant implications for the well-being and development of children. For instance, young people may struggle to access timely and appropriate care due to a lack of awareness or difficulty navigating the existing healthcare system. Additionally, many children and young people are unable to access integrated health services because their conditions do not meet the criteria for existing services.
Child Health Inequalities – Food and Fuel Poverty:
There are significant disparities in child health outcomes, particularly regarding issues such as food and fuel poverty. These inequalities can have a profound impact on the health and development of children.
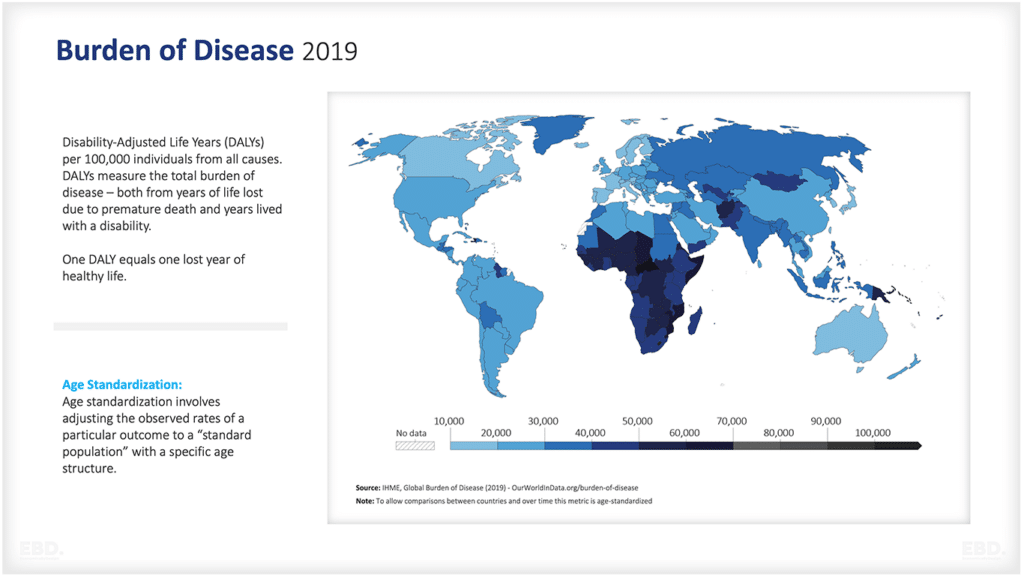
Shift in Disease Burden:
The burden of disease affecting children has shifted from predominantly infectious diseases to a combination of acute and chronic conditions. This change in disease patterns necessitates healthcare systems to adapt and provide appropriate care for these different types of conditions.
Room for Improvement:
Despite advancements in healthcare, there is still scope for improvement in child health outcomes and the quality of care provided. These improvements can be benchmarked against other similar countries.
Quality of Services:
Reviews consistently highlight the subpar quality of healthcare services for children and young people. This indicates a need for systemic changes to enhance the care provided to this population.
Hospital-Focused and Reactive Services:
Child health services often revolve around hospitals and tend to be more reactive than preventive. There is a lack of integration between various services within healthcare systems and limited connection with non-health services that could have an impact on child health.
Health Literacy and Reliance on the Health System:
Limited health literacy within the local populations results in increased reliance on the healthcare system for information and guidance.
Primary Care Challenges:
Primary care, typically delivered by general practitioners, serves as the initial point of contact for most children. However, primary care may lack the necessary resources and time to effectively address the diverse needs of children.
Capability Gap Between Primary and Secondary Care:
There is a noticeable disparity in expertise between primary and specialised hospital-based care. General practitioners may not have access to the same level of expertise as hospital-based paediatricians, which can pose challenges in managing complex cases.
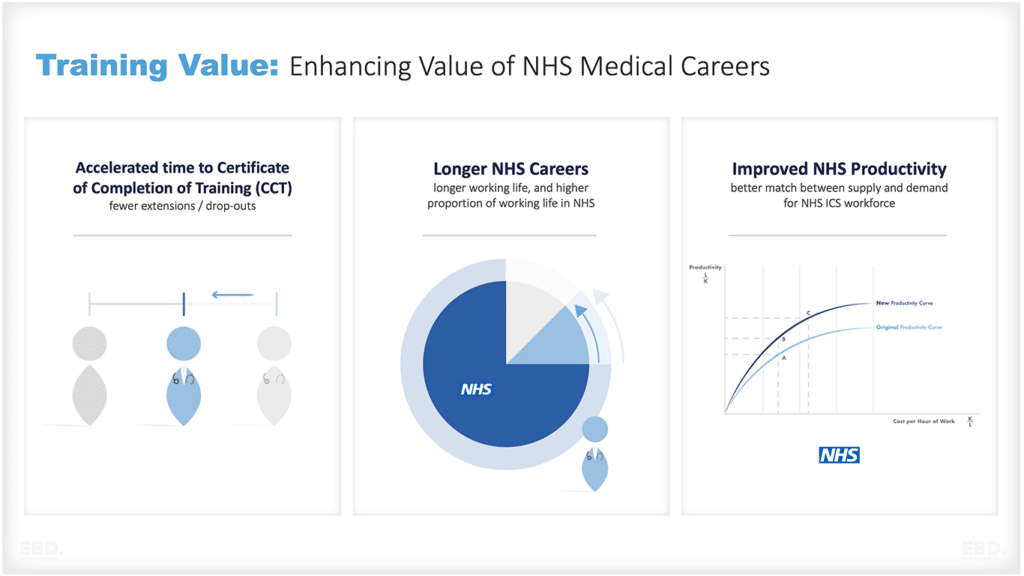
Workforce Planning and Focus on Prevention:
Hospital-based paediatricians may be better equipped to handle acute cases, but they might not receive as much training in prevention and health promotion. This highlights the need for a comprehensive approach to child health that encompasses both preventive and curative aspects.
Integrated healthcare for children: A solution to the challenges
Integrated healthcare for children is important for a number of reasons. It helps to ensure that families receive the right care at the right time, which can reduce unnecessary duplication or delays in treatment. This can lead to improved health outcomes for children and reduce costs associated with fragmented treatment.
Additionally, integration of health and social care services provide comprehensive and coordinated support that takes into account a child’s physical, mental, emotional and social needs. This holistic approach helps to ensure that children can access the care they need when they need it most.
Offering an integrated services approach seeks to address the issues outlined above. Through this system, a range of care services are coordinated and delivered through a single point of contact. This includes primary care, specialist care, health promotion, and education services.
The system is designed to support the wellbeing of children with multi-complex health needs and to increase access to coordinated personalised care. Additionally, it provides parents and carers with a centralised contact for all their healthcare needs within their local communities. This reduces confusion and stress that may arise from dealing with multiple nhs providers.
What is a Child Health Hub?
A Child Health Hub is a localised service for children and their families, providing integrated healthcare services in one single setting. This provides convenience to families and improves quality of care, as it allows patients to access specialist care in their local communities.
The Child Health Hub is designed to improve the health of children and young people through collaboration and engagement of patients, parents, citizens and hospital, community, primary and public health professionals. It facilitates collaborative working between paediatric consultants and GPs to deliver comprehensive care for children in their local communities.
The initial vision for the Child Health Hub, directed by the Connecting Care for Children (CC4C) paediatric integrated care model, aimed to promote seamless integration among primary, community, secondary, and tertiary healthcare services. Additionally, it sought to forge robust partnerships with professionals in various sectors, including schools and social care, to ensure comprehensive support for children’s well-being.
The Child Health GP Hub model brings together nearby GP practices, paediatric consultants, and other healthcare professionals to address the healthcare needs of the local community. With streamlined care and better communication, this model ensures accessible access to specialised services and expertise in child health. Patients benefit from fewer appointments, timely care, and a comprehensive management plan.
An early economic analysis of the initial pilots of the Child Health GP Hub Model in 2012 demonstrated the potential value of this model from a health system perspective. If implemented effectively, this model had the potential to reduce paediatric outpatient visits by diverting them and preventing them through a more integrated and efficient approach. It could also help reduce non-elective inpatient hospital admissions, A&E attendances, and diagnostic tests.
The Child Health Hub service was ahead of its time. It aligns well with the design principles of People Centred Integrated Health Services (IPCHS). These principles include engaging and empowering individuals and communities, establishing strong governance and accountability, reorienting the care model, coordinating services within and across sectors, all supported by an enabling health system.
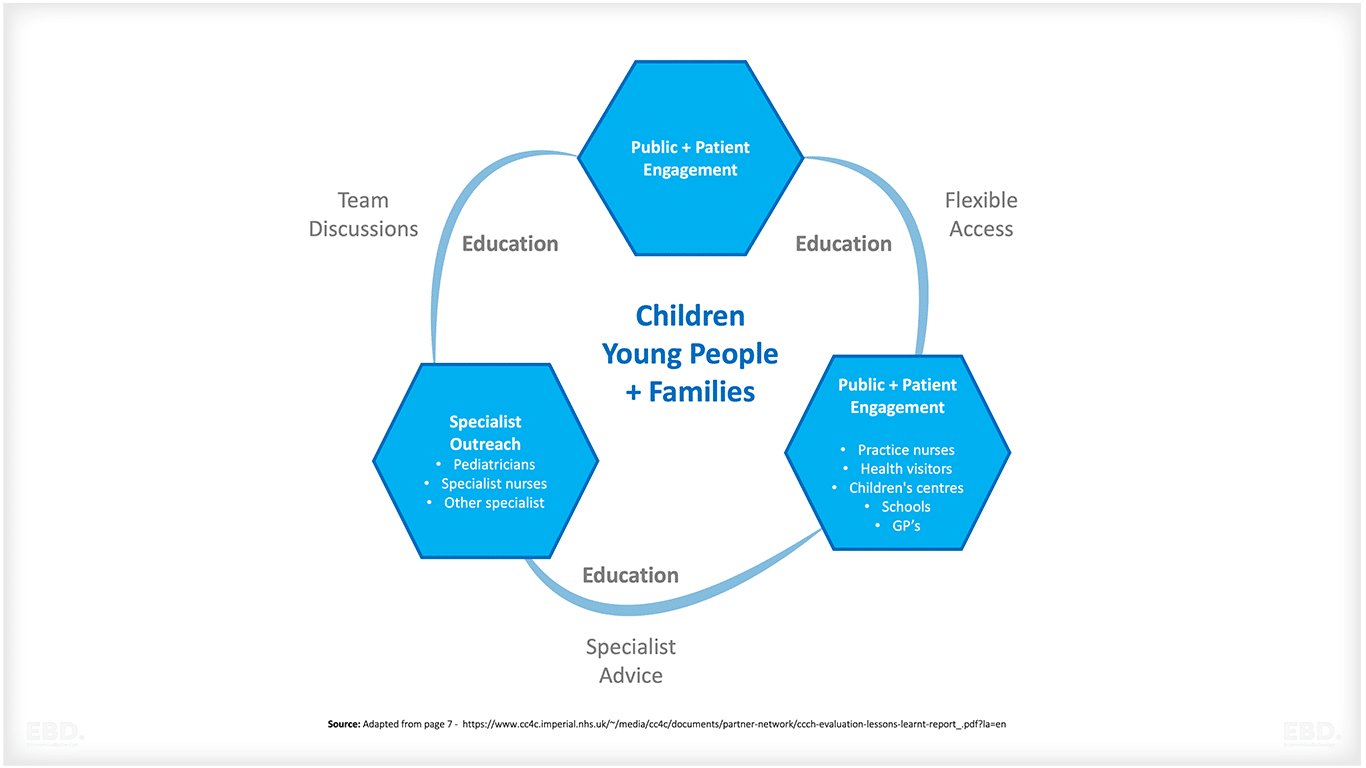
The model comprises of three core elements:
Public and patient engagement:
Involving recruiting practice champions to ensure a focus on local community priorities and implementing a comprehensive public engagement program for health and wellbeing education. This approach aims to enhance the quality of communication, understanding, and involvement with the community, fostering a collaborative and informed environment.
Specialist Outreach:
Comprises monthly lunchtime virtual multidisciplinary team meetings, overseen by a paediatrician. Collaborating with rotating GPs, paediatricians conduct joint clinics at the local practice. Additionally, the GP practice can leverage the expertise of paediatricians for any child health-related matters.
Open access:
Refers to the close interaction between professionals from various disciplines through phone and email. Efforts are continuously being made to expand access for children and young individuals to their GP practices.
The challenges and issues associated with the developing Child Health Hub Model in the NHS
During its inception, the Child Health GP Hub operated within an NHS system that emphasized choice and competition between providers, structured around an internal market. However, this market-driven approach, along with its associated payment models and financial flows, failed to effectively distribute the efficiency benefits of the system among different partners. This hindered the required collaboration by health providers across care settings.
Additionally, the segregated design of the system required special measures to pool budgets, often overlooking the needs of children and obstructing multi-sector collaboration.
The development of the Child Health Hub faced several other challenges and issues. Primary Care Networks vary in size, geographic coverage, and cultural maturity, so spread and adoption required careful planning, starting with those that have already expressed interest.
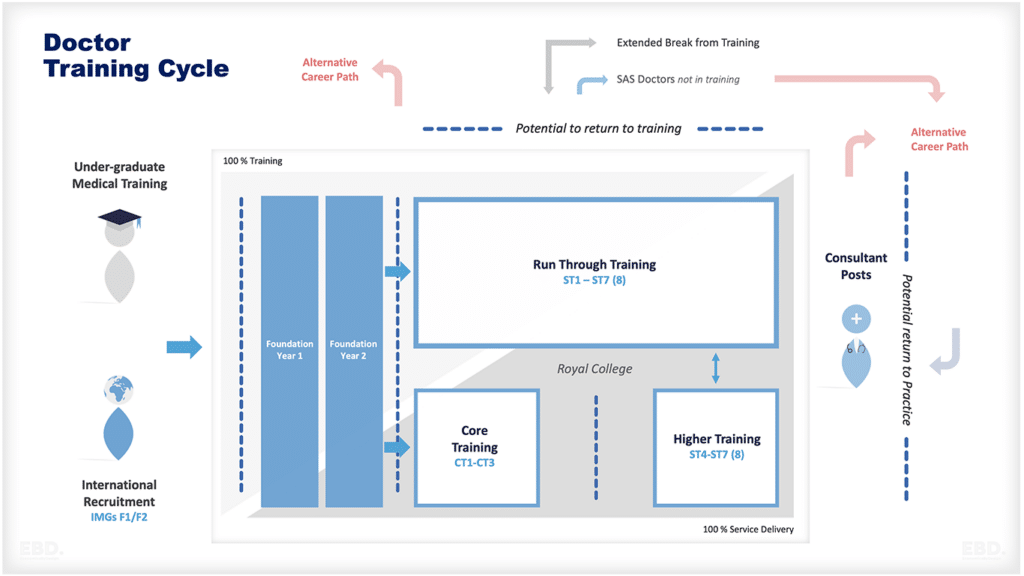
Shortages of consultant staff and general practitioners coupled with the difficulty of reallocating staff from immediate pressures on the system, further complicate the development of a new integrated working model.
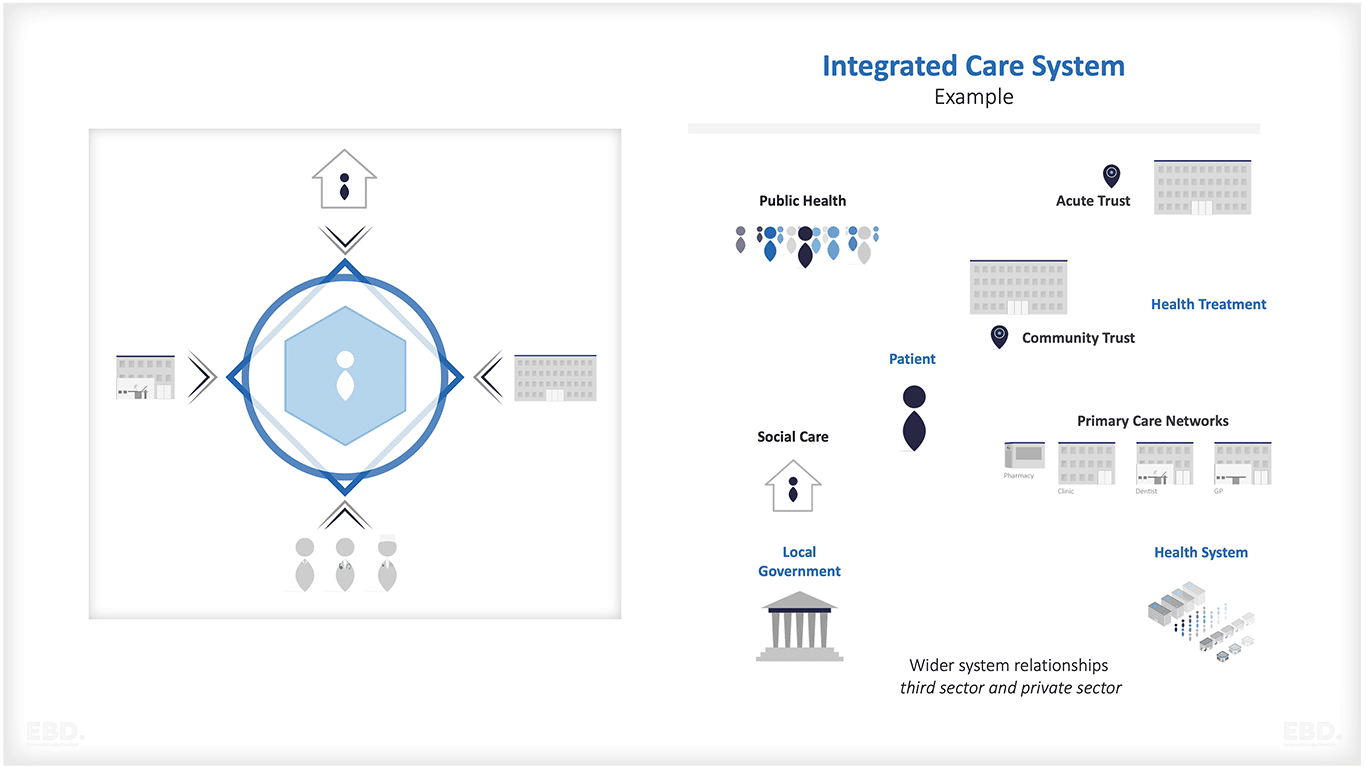
The Enabling Role of Integrated Care Systems
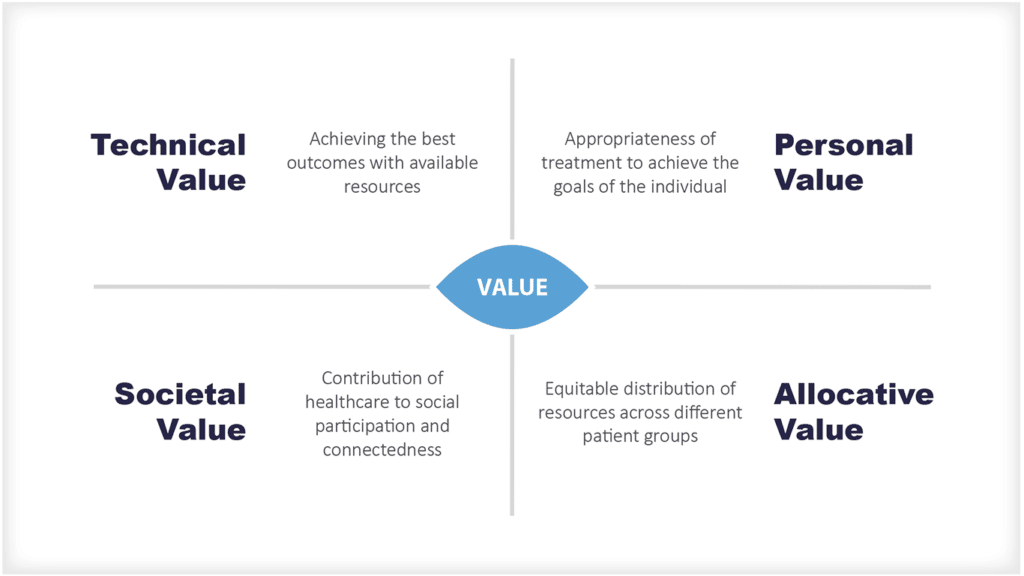
Integrated Care Systems were introduced in the NHS in England as part of the Health and Care Act 2022. At the time of writing there are 42 Integrated Care Systems each existing to achieve four aims:
- Improve outcomes in population health and healthcare
2. Tackle inequalities in outcomes, experience and access
3. Enhance productivity and value for money
4. Help the NHS support broader social and economic development
Many of the challenges and barriers described above are there because of previous system design faults that resulted in misaligned incentives for collaboration and integration. Integrated Care Systems should enable these challenges and barriers to be overcome.
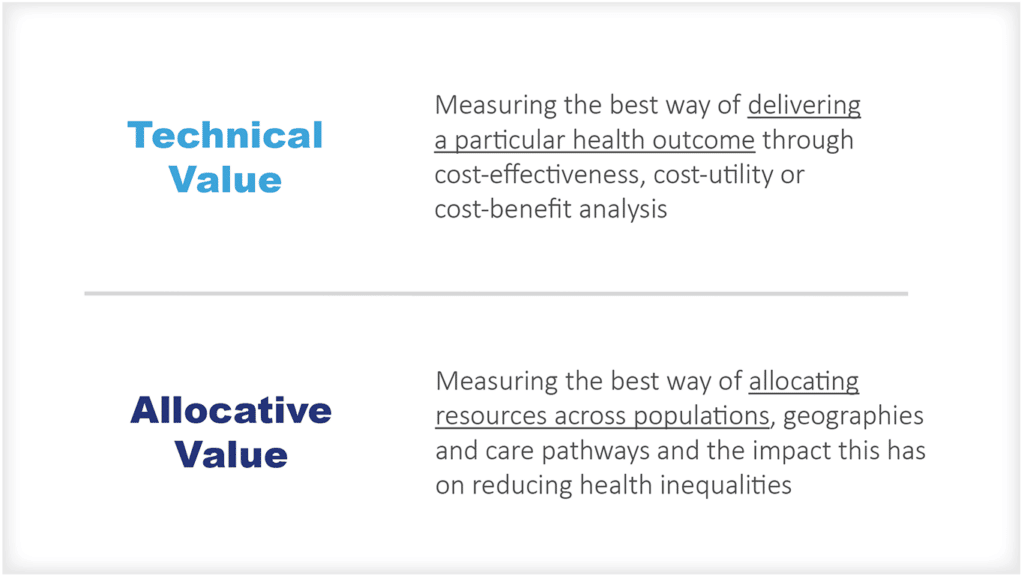
In particular Integrated Care Systems will be given a lot more flexibility to determine how funding flows, than existed under the internal market. As they mature, and use these flexibilities to solve the local problem faced, they will need be able to pay attention to payment models as positive levers for achieving their goals.
North-West London Child Health Hub: A Model Case Study
The North-West London Child Health Hub (NWL CHH) implemented the Child Health GP Hub model in North West London as a development of the connecting children for care (CC4C) project.
The NWL CHH offers timely and effective care for children with complex needs, starting from pregnancy and throughout their childhood. Local services include early years support, emotional well-being, mother and baby mental health, antenatal classes, parenting programmes, education outreach coordination, and health visitor support. In addition, it provides direct clinical care for children with conditions like asthma, diabetes, post-surgery follow-up, dental care, and early intervention for special educational needs.
The NWL CHH has successfully implemented integrated services that address the needs of families in their local communities. It serves more than 100 GP practices in North West London and has achieved a significant reduction in paediatric outpatient appointments, leading to improved health outcomes for children with complex needs.
The success of the NWL CHH serves as a compelling example of how integrated care systems can enhance population health across diverse communities. This model should inspire other regions seeking to implement similar initiatives, aiming to deliver better healthcare outcomes for their local population.
A summary of the benefits of the NWL Child Health Hub Model
- Improved access to local health services for children and young people, as well as their families.
- Streamlined care services provided by multidisciplinary teams in one place, resulting in better quality of care.
- Reduced waiting times and improved health outcomes due to efficient communication and collaboration between specialists and GPs.
- Enhanced public engagement and education, leading to more informed decisions.
- Increased satisfaction from patients due to better coordination and communication with healthcare professionals.
- Cost savings for the health system as a result of reducing hospital visits, A&E attendances, and diagnostic tests.
- Improved care plans that are tailored to individual needs, creating better communication between families and healthcare professionals.
- More efficient use of medical resources with fewer duplicated tests and more integrated services across the sectors.
- Increased capacity for GPs to provide local services to collaboration with paediatric consultants.
- Greater connection between primary, community, secondary, and tertiary health services for a more unified approach to healthcare delivery.
The Positive Impact of Child Health Hubs in North West London
For Patients and Families
Child health hubs provide a range of compelling benefits for patients and their families, as highlighted in a comprehensive report on Child Health Hubs in North West London.
Notably, an astounding 88% of parents express increased confidence in seeking medical care for their children from general practitioners in the future, reflecting the positive impact of these hubs. An integral factor contributing to this confidence boost is the strategic implementation of targeted preventive measures, which have resulted in substantial improvements in population health outcomes.
A prime example of these improved outcomes can be seen in the care provided to children with asthma. Comprehensive care plans tailored to meet the child’s needs across various contexts – including home, school, general practice, and hospitals – have led to a remarkable enhancement in the quality of care for these young patients.
Additionally, the innovative use of platforms like WhatsApp groups has proven highly effective in sharing vital immunization information. The inclusion of informative infographics within these groups has significantly increased immunization rates, highlighting the positive influence of streamlined communication on healthcare outcomes.
In addition to these notable achievements, child health hubs offer a series of patient-centric advantages that greatly alleviate the challenges typically associated with medical appointments. The convenience of timely appointments within a familiar and local environment substantially reduces appointment-related anxiety.
Moreover, the opportunity to consult with specialists in such a setting minimizes practical obstacles like travel and parking, thereby enhancing the overall patient experience.
Patient experience data has been gathered through Patient Reported Experience Measures (PREM forms). In 2019, patients expressed the following sentiments: 79% preferred the GP setting; 92% found the information to be clear; 100% felt that families were involved in decisions; and 100% noted that clinicians collaborated effectively.
For Staff
Child health hubs provide numerous benefits for staff, focusing on enhancing their experience and promoting professional development. These hubs offer valuable opportunities for trainee health professionals to gain hands-on experience and build meaningful relationships.
Active participation in these hubs allows staff members to acquire new skills in managing common paediatric problems, boosting their confidence in applying up-to-date clinical knowledge. Moreover, the hubs empower staff to explore their clinical interest areas, leading to increased job satisfaction.
One pivotal advantage of child health hubs is their ability to improve communication between primary and secondary care. This synergy enables staff to access timely email advice from paediatricians and specialists, facilitating decision-making and reducing the need for repeat appointments.
Additionally, child health hubs foster collaboration with colleagues in the healthcare system, including health visitors, Children and Adolescent Mental Health Services, and social services. This collaboration improves signposting and enhances the utilization of local resources, ultimately benefitting the quality of care provided to children.
For the System
Child health hubs offer a wide range of significant benefits to the healthcare system. Notably, a service evaluation suggests that early versions of the Child health hubs successfully reduced outpatient visits by an impressive 39%, resulted in a 22% decline in accident and emergency cases, and a 17% decrease in admissions.
These outcomes underscore the effectiveness of the child health hub model in optimizing healthcare delivery and resource allocation.
The development of robust care models within child health hubs serves as an exemplary blueprint for other medical specialties seeking similar success. These carefully designed and refined models aim to achieve two objectives: reducing unnecessary referrals and improving the quality of existing referrals through enhanced patient history and thorough workup.
At the core of this approach is placing the patient at the centre of service delivery, shifting the focus from hospital-centric care to community-based solutions. This not only aligns with patient preferences but also fosters a more sustainable and efficient healthcare ecosystem.
The Business Case for The Spread and Adoption of the Child Health Hub
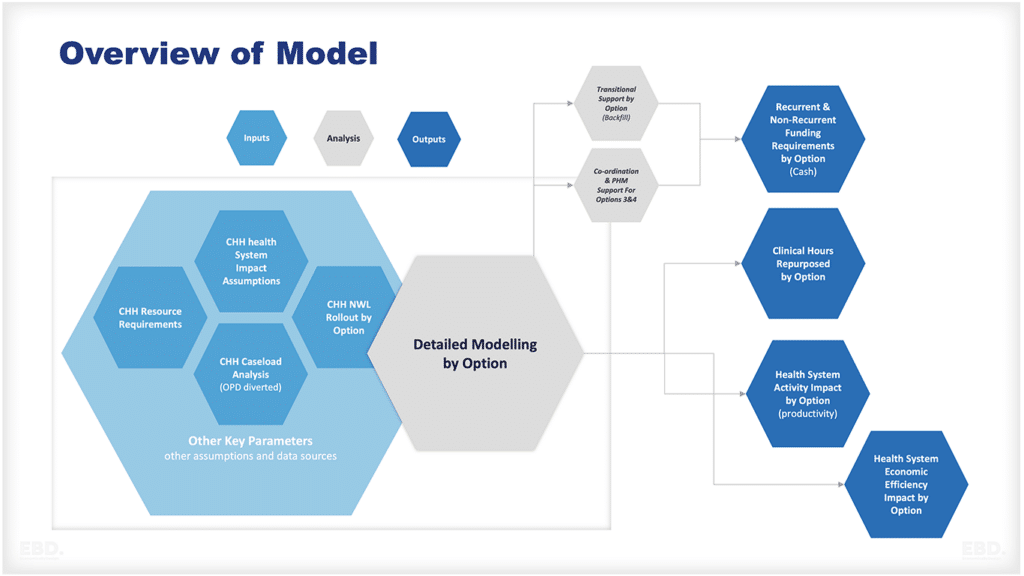
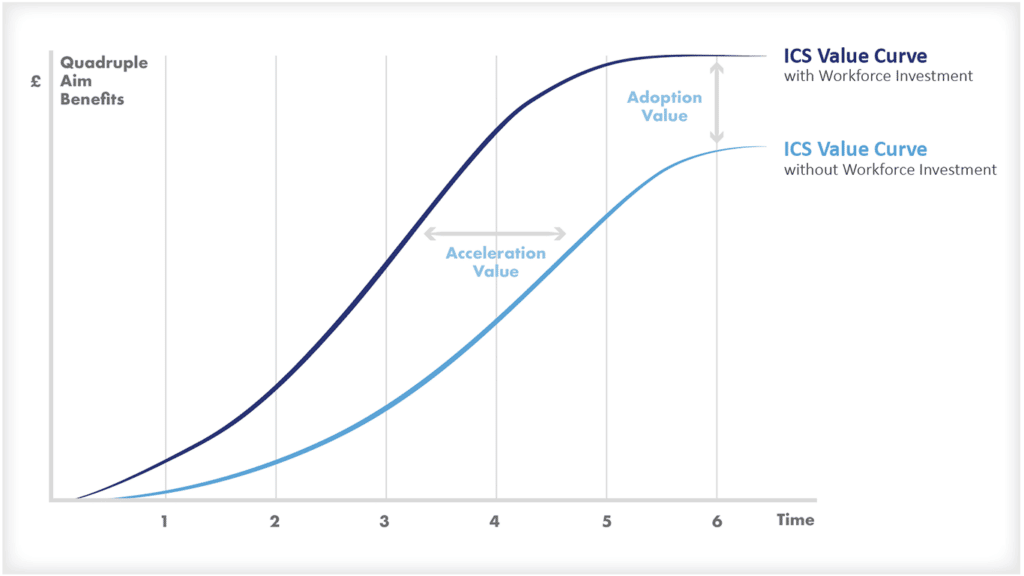
North West London Integrated Care Board recently approved a business case for transitional funding to support the spread and adoption of Child Health Hubs across the system. The business case looked at the case for change, options for developing child health hubs, qualitative and quantitative costs and benefits of the options, affordability, and mangement and benefits realisation issues.
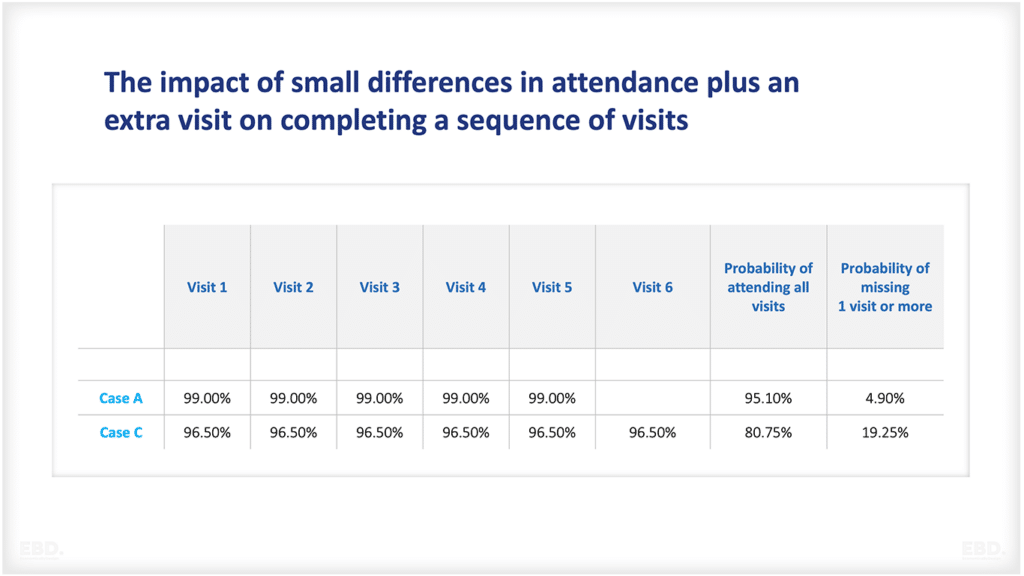
The “value case” prepared to support the business case was based on modest assumptions (compared to previous evaluations) about health system efficiency gains which would be generated from adopting the Child Health Hub.
Specifically that on average they would release net additional capacity of 4% new out patients & 7% follow up out patients appointments, 3% of A&E attendances and 7% of admissions as well as reductions in GP appointments and mental health referrals.
Even these very modest assumptions were sufficient to demonstrate that there was significant net value to be achieved from transitional investment to support spread and adoption.
Other models of integrated care for children and young people
United Kingdom
The CHILDS Framework, South London
The Child Health Integrated Learning & Delivery System (CHILDS), is a comprehensive framework designed to enhance health and care for children. Initially implemented in Southwark and Lambeth, through the Children and Young People’s Health Partnership initiative.
This model aims to prevent hospitalization and provide localized care through neighborhood child health teams. These teams deliver early intervention, health promotion, and integrated care within primary care networks.
The triage process allows child health teams to offer advice and guidance to general practitioners for 45% of cases, refer 31% to integrated child health clinics, 9% to integrated long-term condition services, and make specialist referrals for 13% of cases. As a result, there have been significant reductions in emergency department visits and non-elective admissions.
Population health management plays a crucial role in addressing health equity by prioritizing children with the greatest needs and providing early intervention and care. This data-driven approach follows the principle of proportionate universalism.
The CHILDS Framework has successfully supported children with challenging health and life conditions such as asthma, anxiety/depression, mental health issues, housing instability, and food insecurity.
Battersea PCN, Youth Clinic Fellowship Project, South London
The Youth Clinic, established by Wandsworth PCN, is a holistic clinic located in Battersea that focuses on providing appropriate healthcare and signposting services for the adolescent population. This clinic was initiated as a pilot project based on an existing adult social prescribing service. Its primary objective was to foster a stronger relationship between children and young people (CYP) in Wandsworth and their GPs, as well as facilitate their registration with a GP.
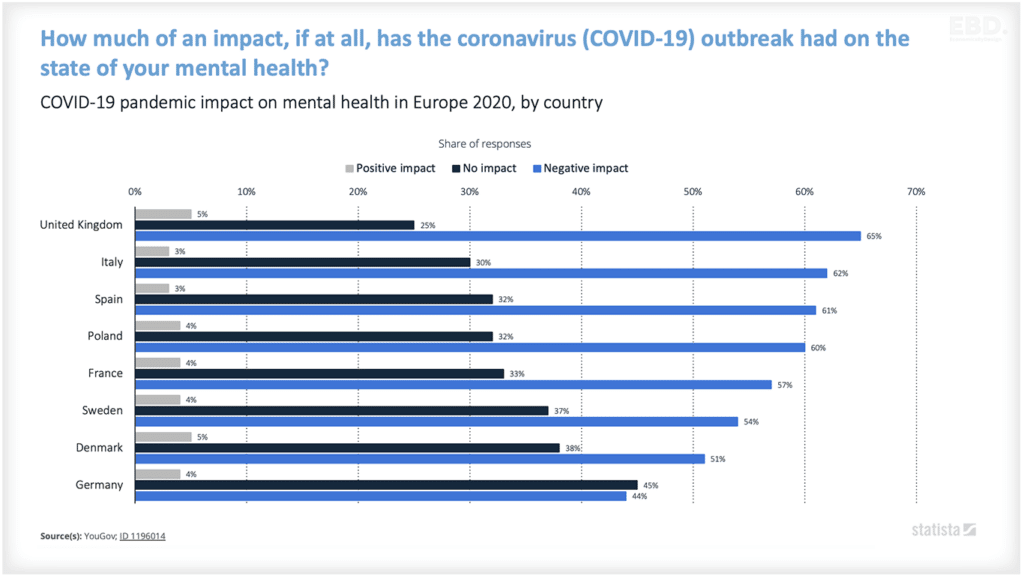
The post-COVID-19 landscape has highlighted an increased demand for mental health and wellbeing services, with a significant number of children and young people experiencing anxiety and depression. An evaluation, conducted over a period of two years, revealed that social prescribing played a crucial role in providing interim support for CYP while they awaited access to statutory mental health services.
Well Centre, South London
The implementation of an adolescent health ‘one-stop-shop’ model is exemplified by The Well Centre in South London.
Developed jointly by Redthread, a youth work charity, and the Herne Hill Group Practice (GPs), The Well Centre offers a drop-in service at the Streatham Youth and Community Trust building. It provides access to healthcare professionals such as GPs, mental health nurses, and youth workers, all working together in an integrated approach to meet the healthcare needs of young people (YP) aged 13-20 in the London borough of Lambeth.
Mental health problems were found to be the most common issue among the two-thirds of children and young people attending the centre, followed by infectious and parasitic diseases and genitourinary system diseases.
Interestingly, a third of the attendees reported not having a GP, indicating that the Well Centre may be bridging the gap in NHS services for disadvantaged individuals and addressing health inequalities in the area.
Health Spot, North East London
The Tower Hamlets GP Care Group and Spotlight youth service have partnered to create a comprehensive youth-centered initiative, known as the Health Spot service. This service offers a holistic health clinic that is accessible to all individuals between the ages of 11 and 19 (or up to 25 for those facing additional challenges like SEND).
Despite coinciding with the onset of the COVID-19 pandemic, the service successfully commenced operations. In its first 10 months, the Health Spot service catered to 51 young people, with many attending multiple times.
The outcomes of the first 51 consultations at Health Spot included various forms of support such as advice, education, referrals, direct medical assistance (e.g., prescription issues), and follow-up options. Patient feedback for Health Spot has been overwhelmingly positive, with 100% stating that they would recommend the service to a friend. Notably, the service was praised for being helpful, friendly, and comfortable.
Integrated Paediatric Service, North Central London
The IPS Model encompasses three primary functions. Firstly, it involves consultant-led triage of general paediatric outpatient referrals. Secondly, it facilitates monthly multidisciplinary team meetings (MDMs) which provide paediatric advice, guidance, and learning. During these meetings, case referrals are discussed by a consultant paediatrician and a team of multi-disciplinary professionals. Lastly, joint primary care clinics are established for selected paediatric cases identified through consultant-led triage.
Currently, 22 Primary Care Networks (PCNs) across 5 NCL boroughs actively participate in either an integrated clinic or MDM model.
Notably, MDMs have seen significant discussions surrounding mental health, with professionals from 14 different agencies attending, including paediatricians, GPs, health visitors, CAMHS, and social prescribers. After MDMs, 39% of children and young people (CYP) have been redirected from trust outpatient appointments, and 18% have been discharged.
Moving forward, the model’s development will focus on obtaining better quality data through Quality Improvement (QI) methodology and Plan-Do-Study-Act (PDSA) cycles. This will allow for a comprehensive analysis of conditions and identification of the most suitable children to undergo this model of care.
Hampshire and the Isle of Wight
A report outlines the successful implementation and lessons learned from the introduction of the Child Health Hub Model by the Hampshire and Isle of Wight Sustainability and Transformation Partnership. It provides an overview of the CC4C Child Care Hub model.
The report presents financial considerations for implementing the Child Health Hub model in GP practices. Furthermore, it shares quantitative data from the pilot implementation of the Child Health Hub model in Chandlers Ford Primary Care Network (PCN), indicating a 13% reduction in GP appointments for children and young people (CYP) over a year, along with a 6.96% reduction in non-elective admissions and a 3.11% reduction in A&E attendances.
Additionally, qualitative feedback from patients and healthcare professionals involved in the pilot hubs highlights the benefits of shared learning, interactive working, and patient-centered care.
The report acknowledges the challenges encountered during the project, including issues with data collection and the inability to fully assess the impact and engagement of primary care providers. However, it also identifies opportunities to further identify and develop future Child Health Hubs, emphasizing the importance of focusing on prevention, well-being, and mental health.
Southern Health and Social Care Trust
In Northern Ireland, two of the five healthcare trusts have implemented the CC4C Child Health GP Hub model. Clinicians have provided positive feedback regarding MDT and Clinics. The majority of MDT attendees have expressed that it has had a significant impact on their patient interactions and has improved their relationships with primary and secondary care.
International Models
Australia
Children’s Health Queensland Hospital and Health Service (CHQ) is dedicated to implementing modern healthcare delivery models to enhance the well-being of children and their families.
The CHQ Strategic Plan 2020-2024
The CHQ Strategic Plan 2020-2024 Outlines the vision is to deliver life-changing care for children and young people. The plan is centered around four key strategic objectives.
- Valuing inclusivity
- Achieving excellence in all aspects
- Promoting innovation and knowledge generation
- Fostering collaborative care.
As of the strategy, CHQ has already implemented several initiatives:
Project ECHO
Project ECHO is a virtual knowledge sharing model that connects professionals to provide support for children and young people. Through interactive conversations and case discussions, ECHO networks facilitate collaborative learning and bridge gaps to drive positive change. Since 2016, Project ECHO in Australia has emerged as the largest hub, establishing networks in areas such as paediatric palliative care, mental health, disability, and more.
General Practice Liaison Program
The General Practice Liaison Program improves communication between the community and hospital health sectors. It also supports Children’s Health Queensland staff in promoting new services, developing referral guidelines, and providing education to GPs.
GP Connect
GP Connect aims to enhance access to healthcare services and reduce unnecessary visits to the emergency department. It provides support to GPs in managing children with complex care needs and promotes knowledge exchange between GPs and Children’s Health Queensland.
By offering increased access to non-urgent support, it encourages the use of alternative pathways to the emergency department. GP Connect leverages existing hospital services to deliver an integrated model of care.
The Integrated Management of Childhood Illness (IMCI) strategy
Developed by WHO and UNICEF, aims to improve access and quality of care for newborns and children in primary health services. It focuses on enhancing health worker skills, strengthening the health system, and promoting healthy family and community practices. The goal is to prevent and manage common childhood illnesses, including those in the newborn period, while supporting healthy growth and development in children.
Angola: Case Study of IMCI:
Efforts to improve child health in Angola have been significant, but child mortality rates remain high. The Ministry of Health, supported by the World Health Organization, is implementing a Training of Trainers program to enhance healthcare services and reduce child and neonatal mortality.
The training aims to strengthen the skills of health technicians and improve indicators such as nutritional status and vaccination compliance. The Integrated Management of Childhood Illness (IMCI) approach is being implemented, using algorithms and manuals to detect and classify illnesses and monitor child development.
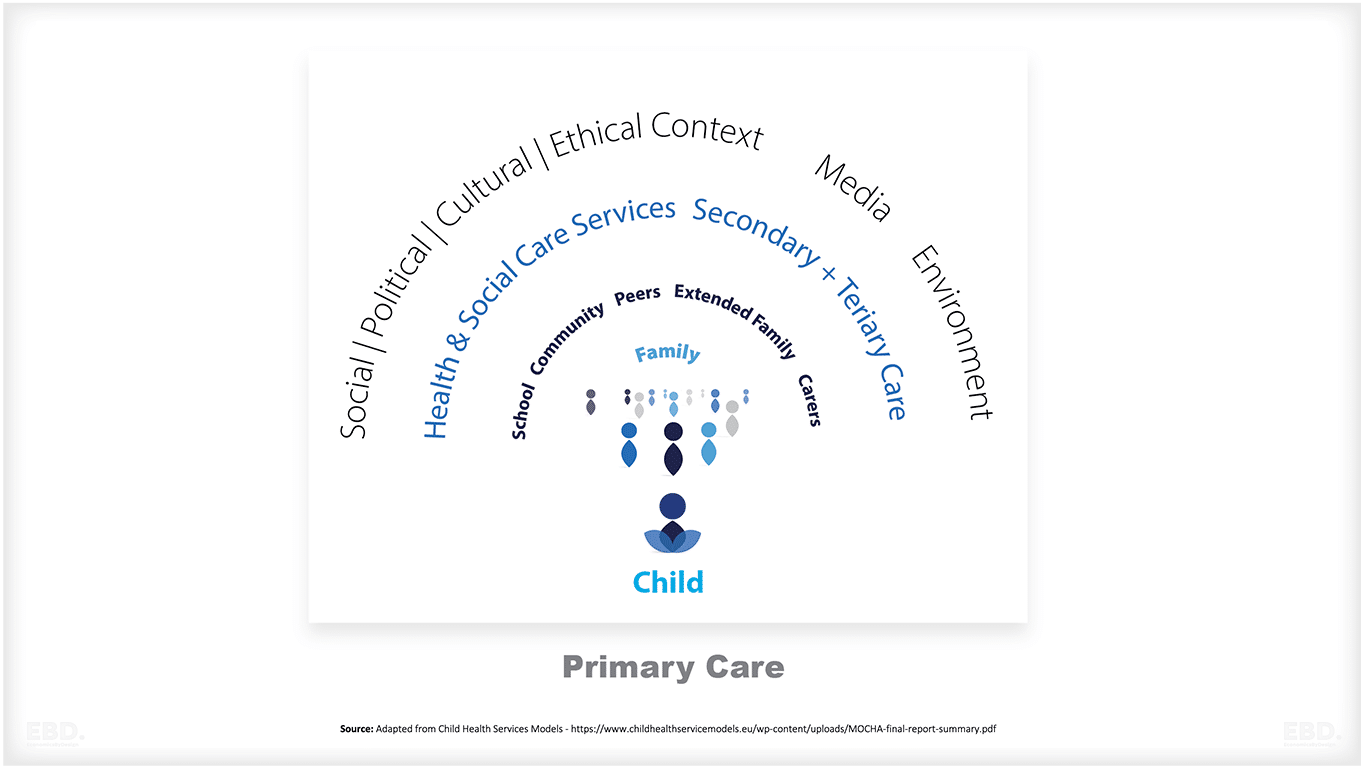
The MOCHA project (2018) undertook a thorough analysis of the various models of child primary health care implemented across Europe over a span of three years. This comprehensive assessment covered all 30 EU/EEA countries.
Consequently, the MOCHA project reached six key conclusions concerning these models:
- The effectiveness of a primary care system depends on factors such as accessibility, capacity, and relationships, rather than the specific style of primary care practitioner, whether general or paediatrician.
- Effectiveness is primarily determined by access, workforce, service coordination and continuity, inter-sectoral governance, sociocultural linkage, and financing.
- Providing optimal primary care for children involves a child-centric approach that is fair, proactive, and seamlessly integrated with specialist, social care, and education services.
- There is insufficient attention given to public health, primary care, and inter-sectoral collaboration when it comes to the concerns surrounding child health and development.
- Children are underrepresented in health data and policy innovation in Europe.
- Increased cross-Directorate and inter-agency collaboration within Europe would enhance the evidence base and policy framework, facilitating the development of robust national systems.
Conclusions
The business case for the Child Health Hub revolves around its innovative approach to delivering comprehensive paediatric care across all care settings. This model focuses on integrating services across various healthcare levels, including primary, secondary, and tertiary care, thereby ensuring seamless coordination and improved care outcomes.
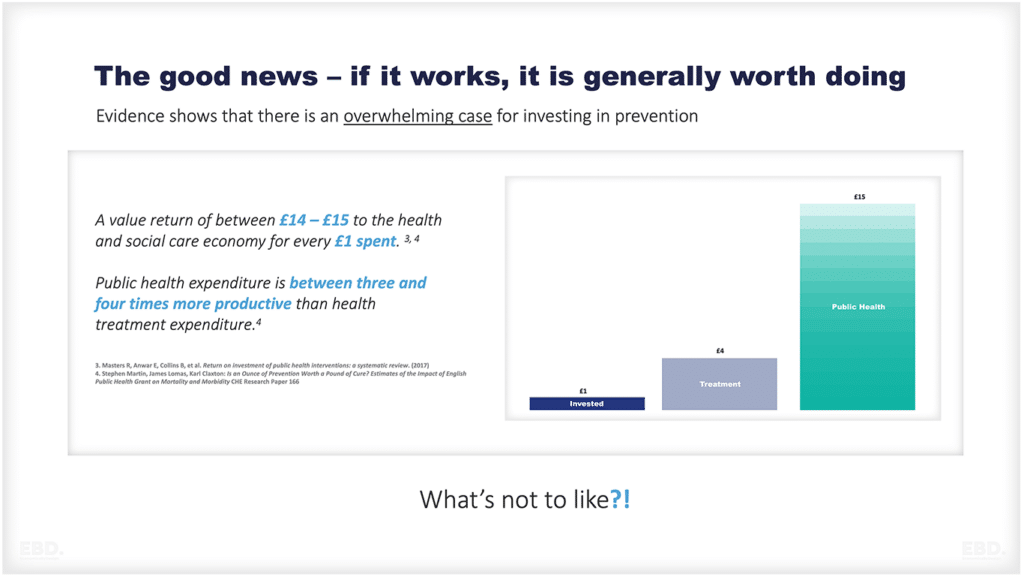
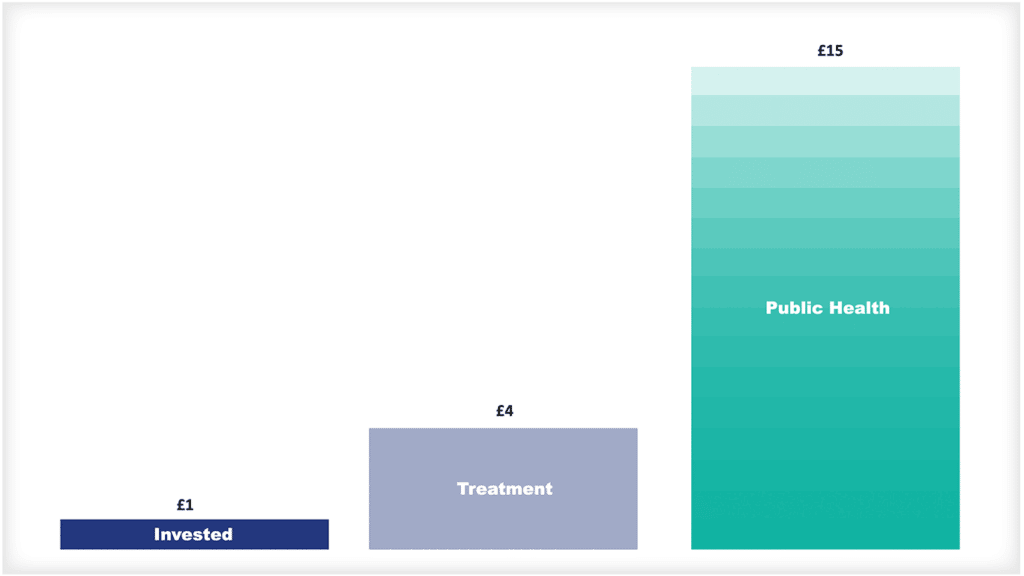
Crucially, it adopts a preventative stance and early intervention strategies, proactively managing common childhood illnesses rather than merely responding to them. This approach is not only more effective and efficient but could also reduce actual healthcare costs in the long term.
Moreover, the hub fosters collaboration and knowledge sharing among professionals, enhancing the overall standard of care. By transforming the healthcare landscape and ensuring equitable access to quality care for all children, the Child Health Hub stands as a financially and socially viable model for improving child health outcomes.