Health Inequalities
Since Marmot (M. Marmot 2010) raised the correlation between social status and health, Health Inequalities has become a major focus.
A decade later, things were even worse (M. Marmot 2020):
‘Inequality increased quite markedly – life expectancy is improving for the top 60%, not for the bottom 40%. More than that, for females in the bottom five deciles of deprivation, life expectancy declined.’
We can observe the staggering scale of health inequalities and health differences experienced by different communities. However, although the symptoms are clear, we lack a theory to connect the massive differences in healthy life expectancy to specific mechanisms.
Given the NHS’s stated anti-discrimination intent and the amount being spent to mitigate Health Inequalities, it would be nice to find out if differences thought too small to account for the inequalities, might aggregate to the disparities observed.
I suspect that major disparities between deprived and thriving communities grow out of very small added barriers experienced by those in the deprived communities. These added barriers result in extra engagements compared with ‘mainstream’ NHS users. This theory is a reasonable one but getting the numbers right is still some way off.
In this article I explore whether it is possible to develop this theory into a model, what we already know and don’t know about health inequalities, and what my personal experience as an expert patient tells me.
Can we build a model of health inequalities?
Here’s a story from one of my favourite thinkers, the Nobel Laureate Richard Feynman, (Gleick 1992, 367). Feynman knew about theory and data, having developed new theories himself. He was also interested in Mayan culture. Here is his Mayan parable.
One day a Mayan astronomer is approached by a chap with a new theory. This chap starts talking to the astronomer about huge rocks that are attracted to one another and occasionally orbit between one another and a central star illuminating them. He believes this may explain eclipses.
The astronomer is sceptical but fair and so he asks the innovator to predict an eclipse. Of course, the chap with the new theory has no chance – there are too many unknowns. Mayan astronomers, however, could predict eclipses with ease, so he sends the chap on his way.
This parable bears reflection in our data-rich era, especially when good theories are hard to find.
Conversely, it is worth reflecting on how many poor theories we have where there are lots of numbers to back them up. In articles about the social determinants of health, for instance, it is not difficult to find tables apportioning the inequalities burden across specific categories of deprivation. Where the percentages come from is not clear to me.
Although Feynman conceived the story to probe the difference between theories that were essentially look-up tables and those based on testable mechanisms, it highlights the choice between data that gets the right results but lacks explanatory power and good theory that lacks appropriate data.
What do we know about health inequalities?
Good healthcare is about long-term engagement and continuity of care
We know that good health is not about isolated episodes of healing but about long-term engagement and continuity. So, let us focus on patients who present at a consultation, which will rarely be a single visit for diagnosis and/or treatment but may involve, say, 5 visits: one or more GP consultations, outpatient consultations, and a procedure and follow up visit.
Health inequalities leads to missed appointments
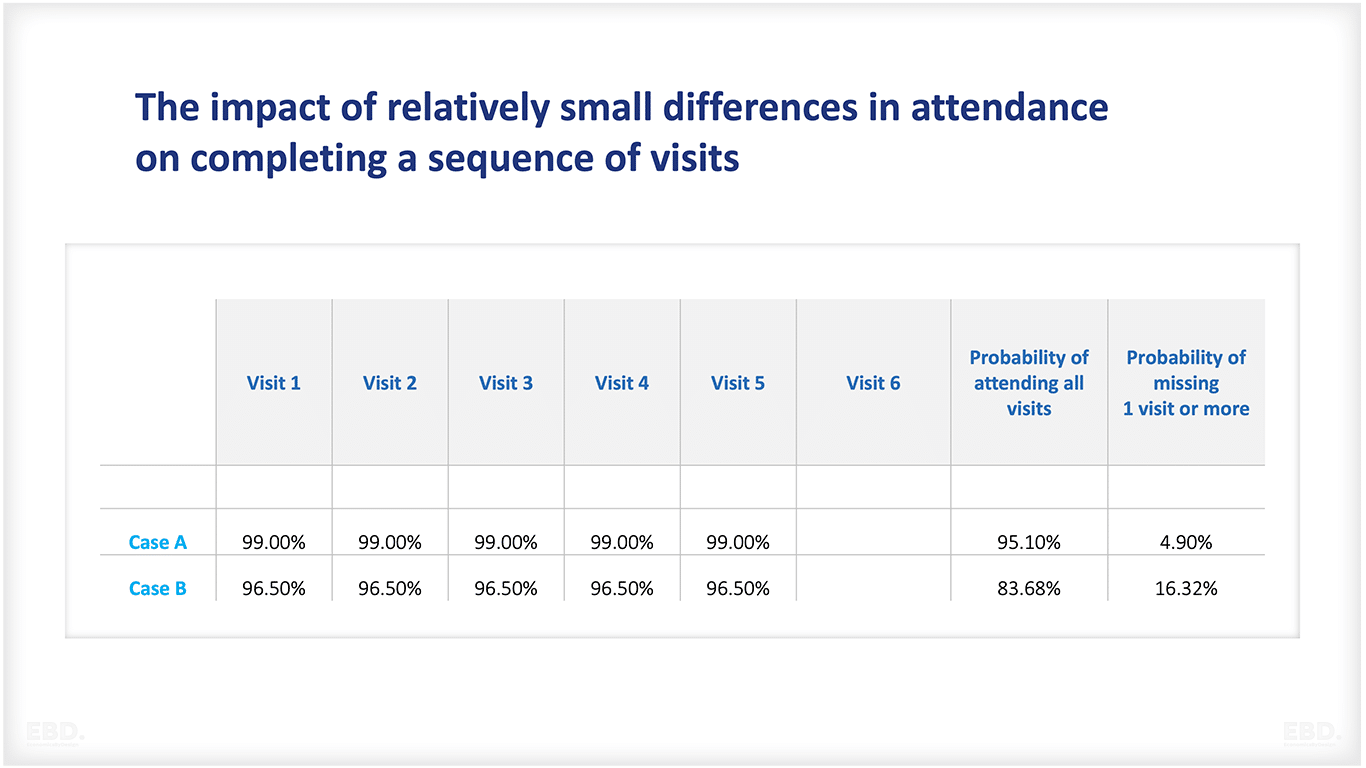
We know that appointments are missed (DNA – Did Not Attend) and that those who experience health inequalities tend to have higher DNA rates (NHS 2023). It is not difficult to show that even if a community is only slightly less likely to attend, the chance of making all 5 appointments falls noticeably.
In Table 1 – a made up example – we have two communities, one that is 99% likely to make its appointments (Case A) and one that is just 2.5% less likely at 96.5% (Case B). Table 1 shows that in our example the likelihood of missing an appointment in the visit sequence rises to around 1 in 6 from around 1 in 20.
Table 1: The impact of relatively small differences in attendance on completing a sequence of visits
Moreover, we know that systems naturally amplify such differences. The slowest checkout, for instance, even if only slightly slower than the rest, will stand out by the much longer queue of waiting shoppers.
What won’t we know until we have data?
The mechanisms that elevate barriers that increase DNAs
If my hypothesis is right, then data would show these barriers are minor or small mechanisms which particularly impact health inequalities. The heightened barriers are not stopping people from fulfilling appointments, just lessening the chance of attendance.
The full impact of missing an appointment
Recently, I tried to rebook an appointment and the system told me that if I rebooked twice, I would lose my appointment altogether. Such policies – and there are many such – would certainly favour those who make almost every appointment every time, but are they enough? So, we need to know if the appointment chain is broken, what are the results? How long are these chains of visits in practice, anyway?
The full impact of missing a critical appointment
Individual visits often contribute little until a specific point is reached such as a diagnosis or start of treatment. The key question is what happens to people who never reach that critical point?
Understanding these issues would greatly assist in building a theory to link a modest number of missed appointments to very large health inequalities.
What I know and you may not
I’m attracted to this theory partly because I belong to one of these Health Inequalities communities. For nearly 60 years I have walked on artificial limbs provided by the NHS because of a congenital long-term condition.
I’ve never sensed a wave of discrimination; quite the reverse, and almost every individual I’ve engaged with has been helpful and pleasant. However, the system has not always supported the successful and fulfilling life that I’ve enjoyed. Nice people, difficult system.
Here are two examples.
Multiple venues for the same purpose:
When we moved house a couple of years ago, the system needed fresh scans and images of my skeleton, but the appointments that came through were in more than one radiology department. I was able to phone in and someone grouped them together into one visit. It’s not hard to see how others faced with this challenge may not have received a full set of images.
Poor quality appointment information
After waiting an hour for an appointment with a specialist clinic and discovering that the information I received was what people hoped was happening rather than what was happening, and that I still had a long wait, I re-booked for the earliest slot on a later day and left in time to make my lunchtime appointment.
Neither of these is particularly unusual, but both add to the challenge of keeping appointments. My guess is that for each community experiencing the downside of wider determinants of health, there will be a host of small factors that add up to slightly higher barriers and slightly lower chances of making the next appointment.
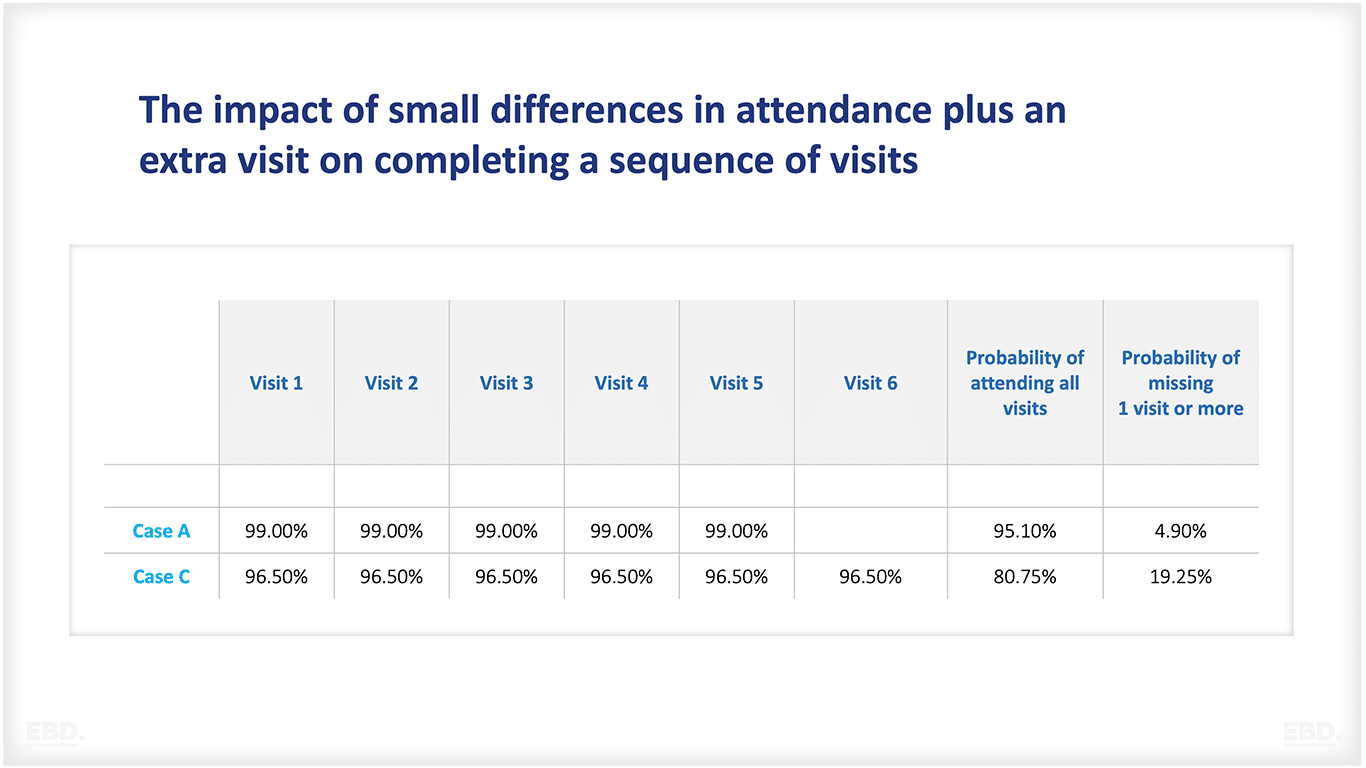
There is something else from this story: I must fit in more appointments than other people. If we add an extra visit to our picture from Table 1, Case C, a very modest increase, Table 2 shows us that failure to complete the full set falls to nearly 1 in 5 (Case C) from the initial 1 in 20 (Case A).
Table 2: The impact of small differences in attendance plus an extra visit on completing a sequence of visits
A final factor from my experience is that the NHS is almost, but not quite a universal care provider, and the breaks in provision often have a disproportionate impact where barriers are already elevated.
In my case, the NHS provides legs, but not crutches. It’s complicated, but basically if you have elbows and hands, off the shelf crutches are available; if you don’t, under the shoulder crutches are no longer provided. Again, NHS staff have helpfully connected me to alternative providers, but it still raises barriers for me.
All this is by way of explanation, not complaint. I am fortunate to have lived when and where I have, and the barriers I’ve faced have not kept me from what I value most.
Summary
We have explored an explanatory model of Health Inequalities in terms of incremental barriers to engagement and slightly higher levels of DNAs in key communities. If this approach is correct, then the system itself serves to amplify these small differences at a micro level into serious disparities across the population.
This simple model is based partly on statistics and the behaviour of systems together with a degree of personal insight gleaned over more than 50 years of experience as a long-term service user.
The big question is: will this idea motivate a search for data with which to build a full theory?
References
Gleick, James. 1992. Genius: Richard Feynman and Modern Physics. London: Little, Brown and Co.
Marmot, Michael. 2010. Fair Society, Healthy Lives – The Marmot Review. https://www.instituteofhealthequity.org/resources-reports/fair-society-healthy-lives-the-marmot-review/fair-society-healthy-lives-full-report-pdf.pdf: Institute of Health Quality.
Marmot, Michael. 2020. “Health equity in England: the Marmot review 10 years on.” BMJ 368.
NHS. 2023. Reducing did not attends (DNAs) in outpatient services. 15 August. Accessed January 16, 2024. https://www.england.nhs.uk/long-read/reducing-did-not-attends-dnas-in-outpatient-services/.