Health Informatics And Information: An Overview
Health informatics, health information and health data are an important and valuable asset for patients who need to know about their own health status and treatment options, staff working in health delivery roles who need to ensure the individual patient receives timely care and treatment appropriate to their needs, staff with management responsibilities who need data to inform how they should target resources to where it is needed, and health system leaders who need to ensure effectiveness and efficiency for those paying for health services.
In this economic lens, we provide an overview of health data and health informatics, how it is used, how it is governed and where it can add value.
Health informatics can be informed by a variety of data about the economy, infrastructure, and many other determinants of health and health system performance. This article focuses on data about the health status and health care of individuals.
What Are Health Data?
According to Health Data Research UK (HDRUK):
“Health data refers to data related to a person’s health; their health conditions, information relating to maternity and children, causes of death, and quality of life. Health data includes, for example: patient health records, studies about the health of groups of people, data from blood or tissue samples, imaging data, and data from health and fitness devices.“
How Are Health Data Collected?
Health data are collected from many diverse sources.
For some individuals, health and fitness devices are increasingly being used to collect basic information about health status, in real time. For others, health data are only available when the individual has a health issue or need for health treatment and data are collected as a result of a specific health test.
When an individual interacts with their health provider(s), health data will be collected insofar as it is relevant to the interaction. Data are collected as part of an appointment, attendance, and admission. Data will be collected by clinicians during a consultation. Data will be collected by a pharmacy, an imaging department, and as part of the preparation for a surgical procedure.
In many low and middle-income countries, health provider data are generally kept as paper records. In high-income countries, these data are increasingly kept in digital form having been collected using information technology systems.
For some providers, information technology infrastructure is linked across departments, so that digital records for the same patient can also be linked, and records can be maintained over time. Some health systems use unique identification to enable information for individuals to be linked across health providers.
How Are Health Data Linked?
To link health data across different digital data capture systems there is a requirement for digital systems to “speak the same language”, or, in other words, interoperability. This may take the form of a common dictionary with shared meaning, known as semantic interoperability. It can also take the form of being able to exchange data between systems.
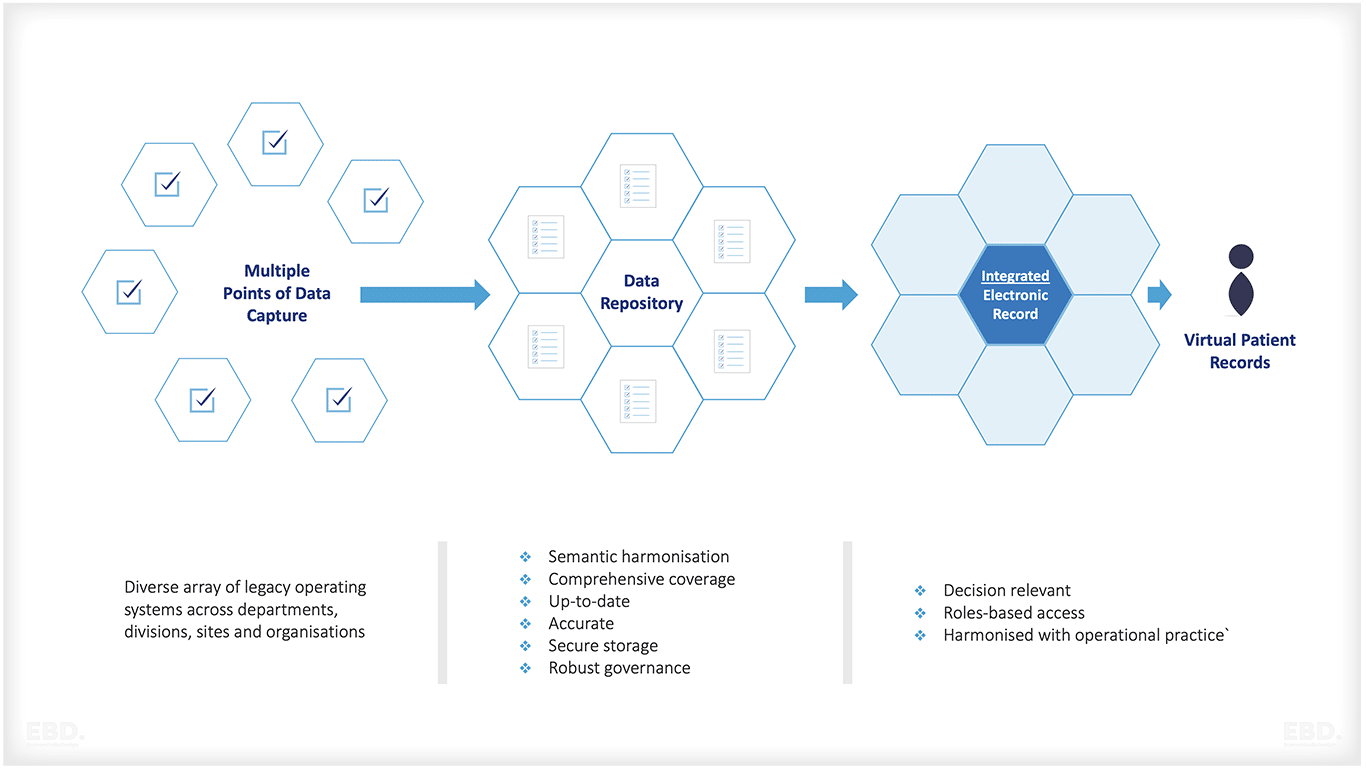
Electronic Health Records
For some health providers, individual patients each have their own comprehensive digital health record or electronic medical record or electronic health record (EMR or EHR). An EMR contains the same information as a paper chart and typically includes patient demographics, progress notes, medications, treatments, vital signs and laboratory data. The EMR will be “fed” data by the various information systems used by the health provider to capture data.
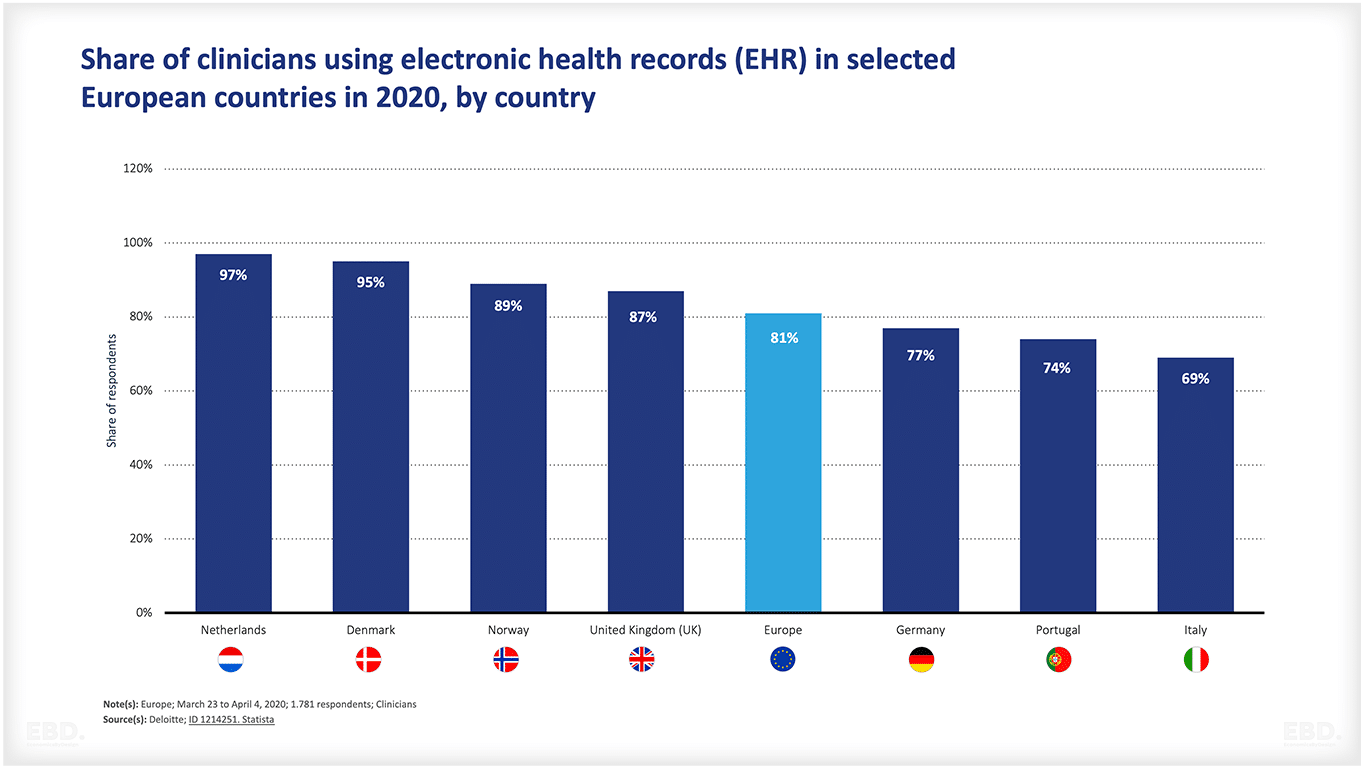
Even across Europe, the chart below shows that there is still considerable variation in the number of clinicians who are using electronic health records.
Inpatient EHR systems are generally used for patients staying in hospitals whilst ambulatory EHR systems are used for patients in primary health care or outpatient settings. Ambulatory EHRs are generally less complex than inpatient EHR systems. In a fully integrated health system, the EHR would enable relevant data to be shared across health settings.
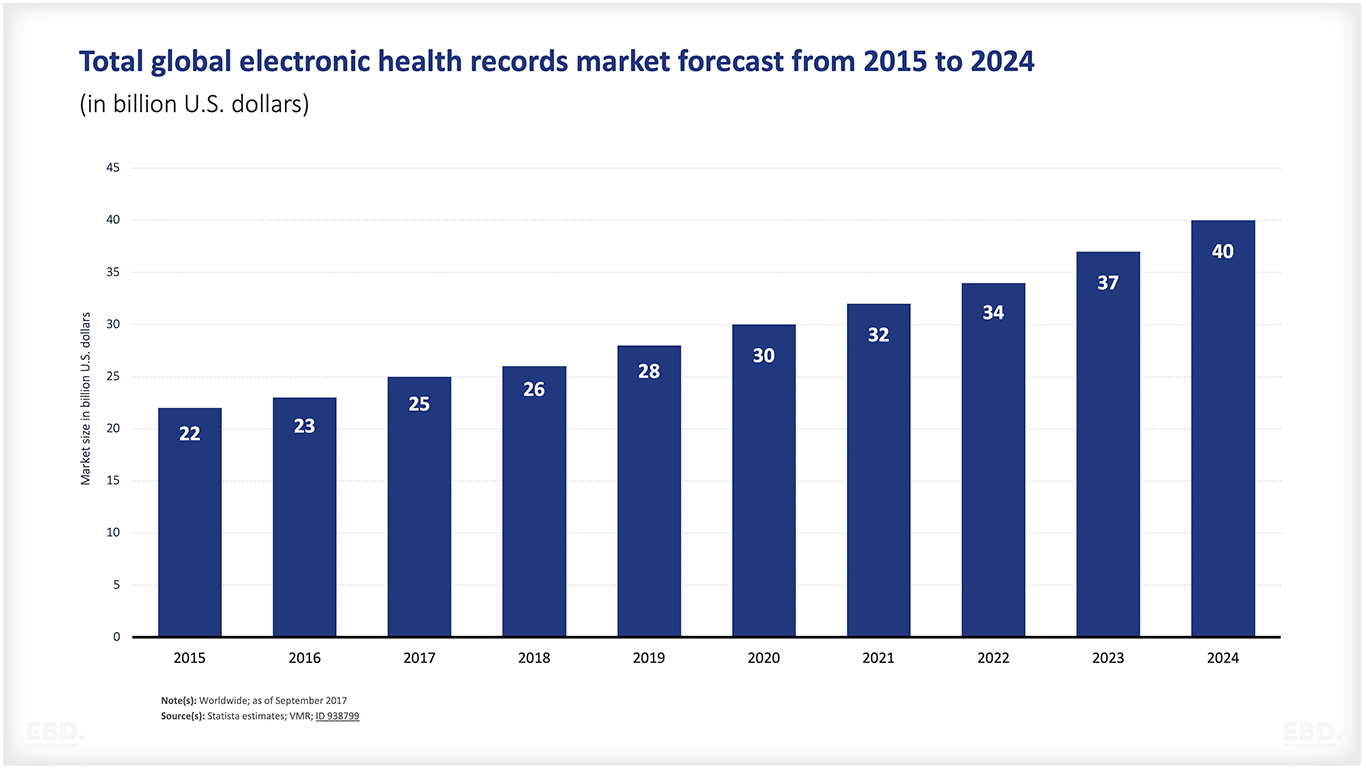
The electronic health records market is considerable. The chart below shows an estimated global value of $37bn in 2023.
The Classification Of Health Information
Health data for individual patients are often diverse, complex and difficult to compare, aggregate or group. For these reasons, health data are recorded using clinical codes, which translate medical information into digital codes that can be recognised within and across digital systems and then aggregated to provide health informatics and related information. Often this is done by a specially trained clinical coder working from paper records and medical notes. Clinical codes relate to pre-defined classification systems set by health insurers, governments and health providers.
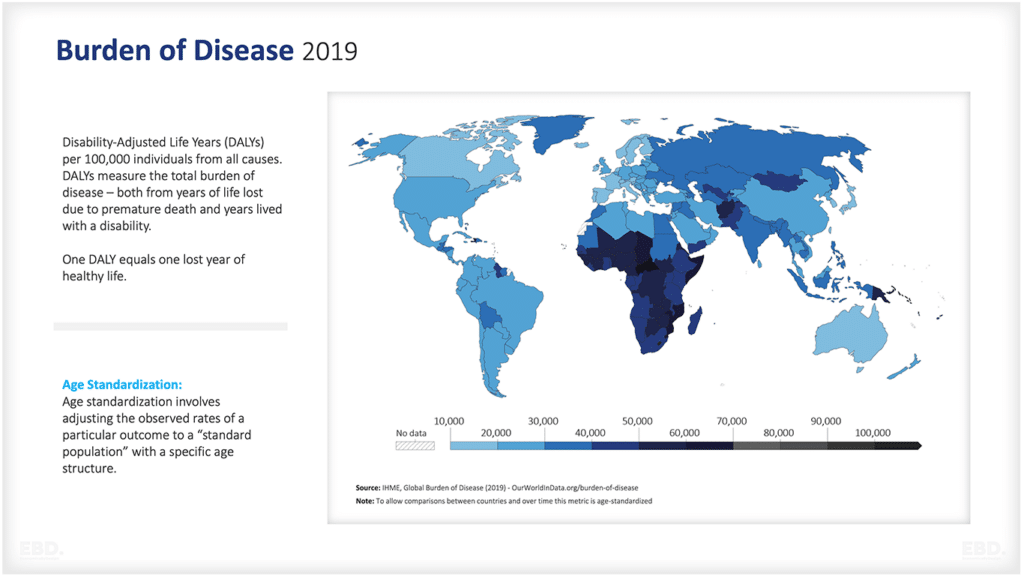
The International Classification of Diseases and related health problems (ICD) published by the World Health Organisation, is used by countries and organisations across the world as a common taxonomy for diseases and death. The ICD system enables in-country analysis of health data and cross-country comparisons. It is a legally mandated health data standard. There have been eleven releases and ICD11 came into effect in January 2022. The WHO also overseas the International Classification of Functioning, Disability and Health (ICF) and the International Classification of Health Interventions (ICHI). Collectively these are known as the WHO Family of International Classifications (WHO-IFC) with the aim of providing one technical language for health workers globally.
Different countries also have their own classification system. The OPCS-4 is a clinical classification system for interventions and surgical procedures used across the four health systems in the United Kingdom (England, Wales, Scotland, and Northern Ireland). OPCS stands for Office of Population Census and Surveys which first published this classification system. In America, the American Medical Association has developed the Current Procedural Terminology (CPT) code to cover medical, surgical, and diagnostic services; the code is used by the Centers for Medicare and Medicaid Services (SME).
Health Outcomes
These classification systems focus on service delivery rather than the actual outcomes of care. In recent years there has been a focus on developing consistent measures of health outcomes. The International Consortium for Health Outcomes Measurement (ICHOM), established in 2012, is focused on developing international definitions and standards for patient-centred outcome measures for a range of conditions and diseases. The outcome measures are being developed based on a hierarchy relating to the health status achieved from an intervention, the process of care delivery, and the sustainability of health as shown in the figure below.
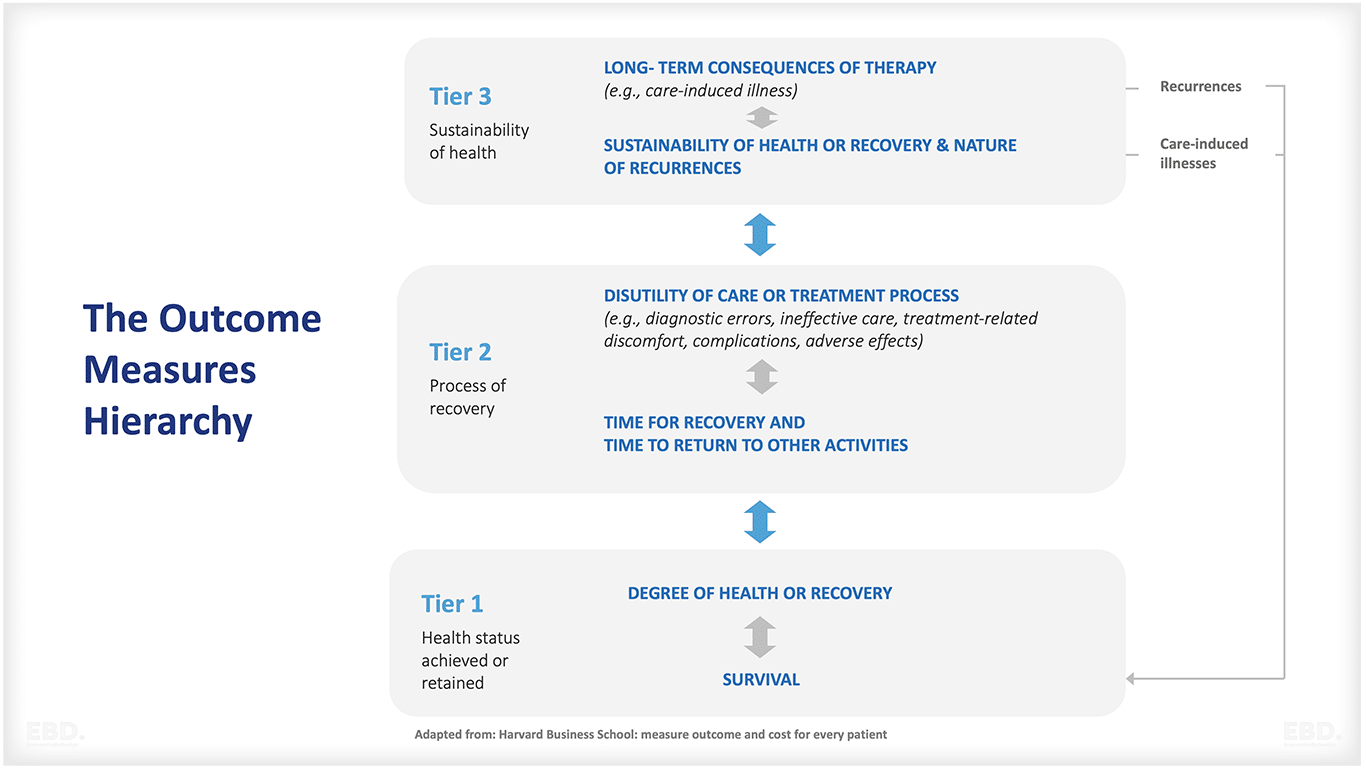
Harvard Business School: measure outcome and cost for every patient
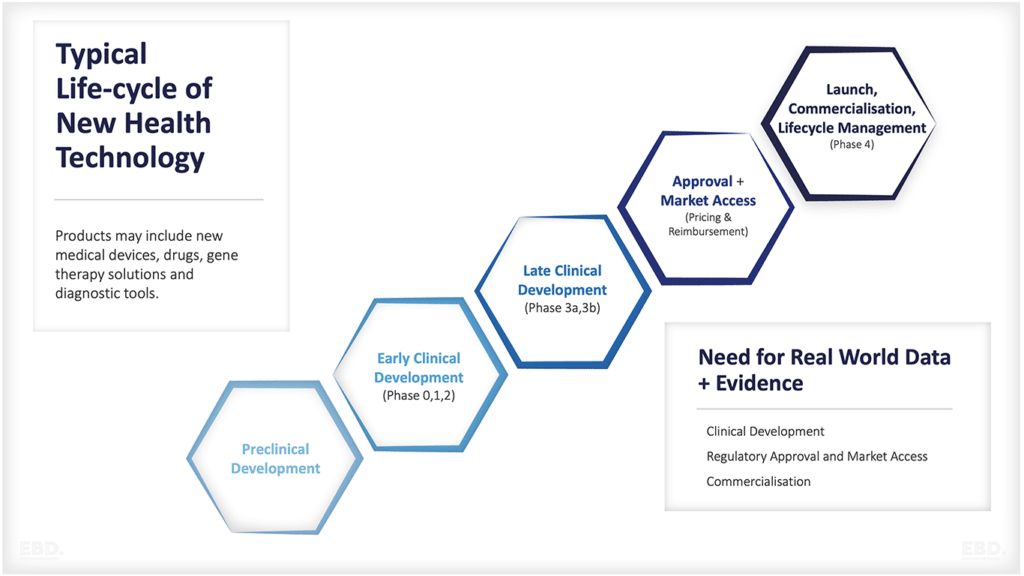
Patient-reported outcome metrics (PROMs) refer to questionnaires or surveys that ask patients directly about their own health outcomes, including pain and disability. This data can be used to measure the effectiveness of treatments or services on patient-reported outcomes in real-world settings. PROMs are now commonly included in clinical trials and research studies to capture a better understanding of how interventions influence patient experience.
Patient-reported experience metrics (PREMs) refer to surveys or questionnaires that ask patients directly about their experiences of care. This can include patient experience and satisfaction with healthcare services, waiting times; levels of communication and information provided by practitioners etc.
Primary Health Data and Secondary Health Data
Primary health data refers to the direct observations and measurements taken by healthcare professionals, such as vital signs, diagnoses and treatments. Secondary health data is derived from primary data sources. It can include an aggregate view of patient populations or a statistical analysis of health resources consumed such as drugs or medical devices used in treatment. In addition, secondary data includes administrative claims and financial data related to healthcare.
What Is Health Informatics?
High-quality health informatics can support effective and efficient patient care, improve public health and population health management, inform health system policy, planning and management, and provide valuable insights for health research and development.
Patient Care
The primary purpose of health informatics is to support prevention, detection, diagnosis, and treatment decisions. Patients and their health professionals can use these data to determine risk factors, analyse symptoms, support diagnoses informed by imaging reports, pathology test results, other diagnostic test results, determine treatment and rehabilitation regimes and, where relevant options for palliative care.
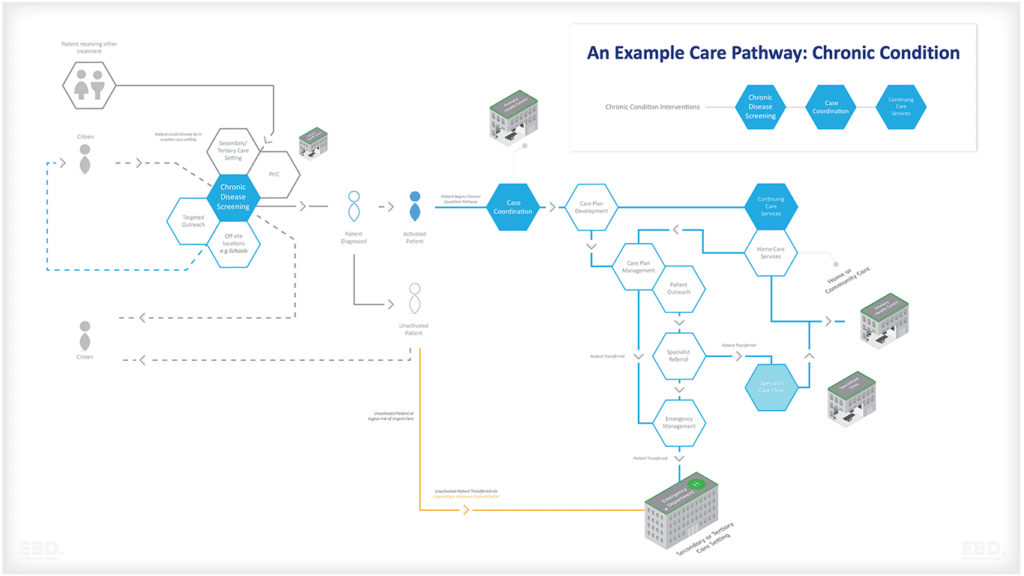
Real-time information about medical history including medication, allergies, and other risk factors can improve patient safety and clinical outcomes. Continuity of information as patients transfer from one healthcare professional to another along a care pathway can increase efficiency and effectiveness and improve the patient experience.
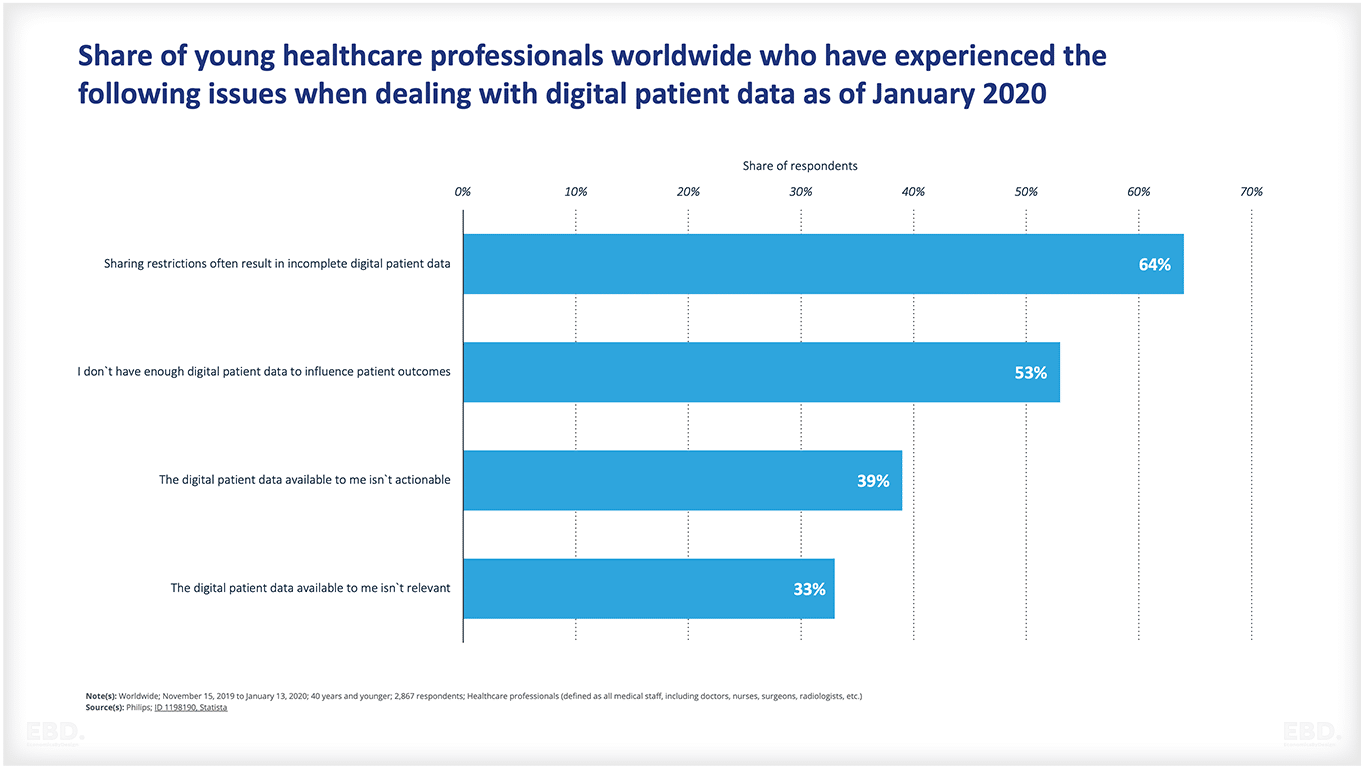
The chart below shows some of the challenges faced by healthcare professionals who want to use digital patient data. The biggest challenges are that records are often incomplete, and may not be directly relevant or actionable.
Population Health Management
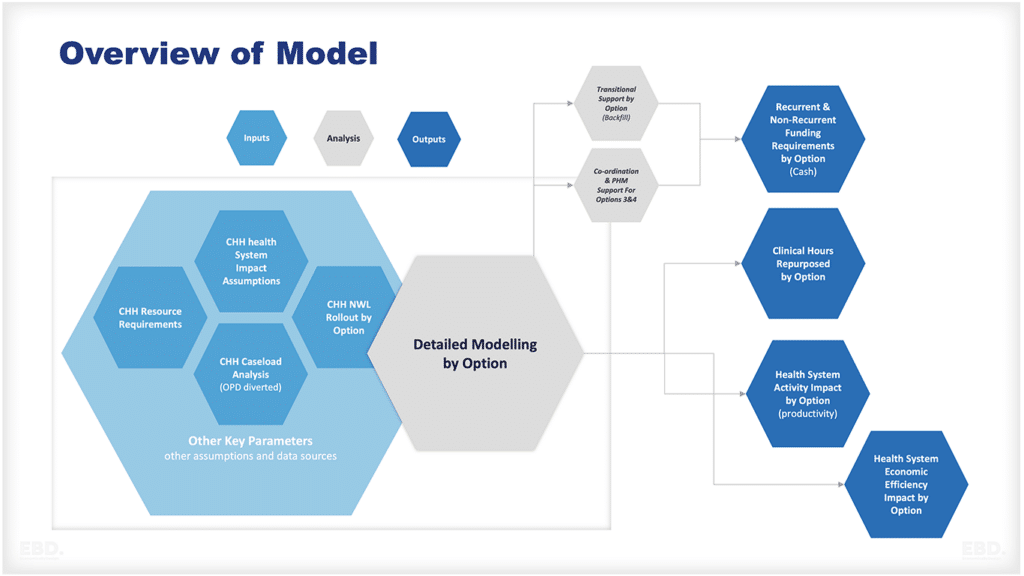
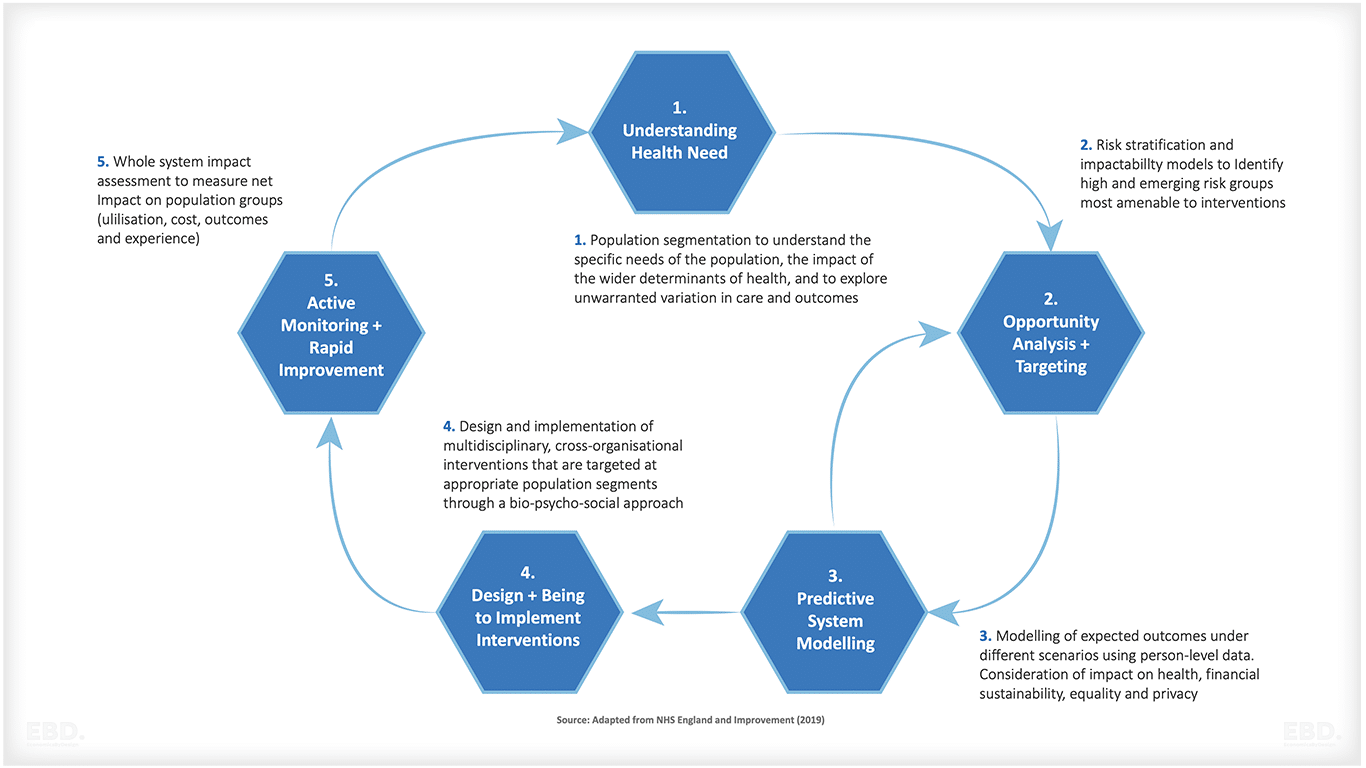
Health informatics can provide insights into population health management and public health initiatives, enabling organizations to identify trends in the prevalence of certain diseases or other conditions and develop interventions that reduce hospital readmissions or improve patient outcomes. This could include finding ways to reach populations who are not accessing healthcare services, developing programs for disease prevention, and improving access to care. The learning cycle of population health management design is illustrated in the figure below.
Health economics of health informatics and data
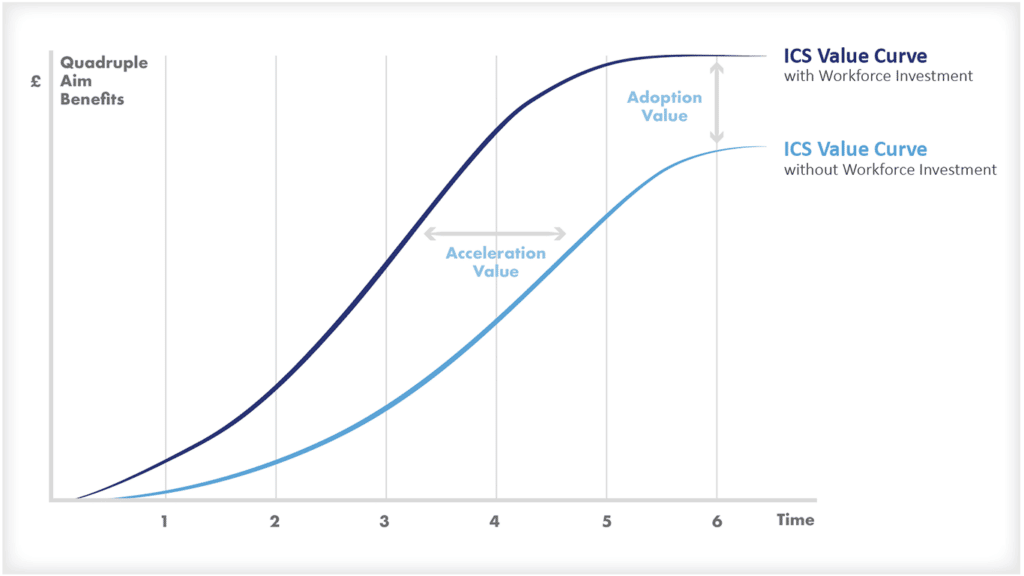
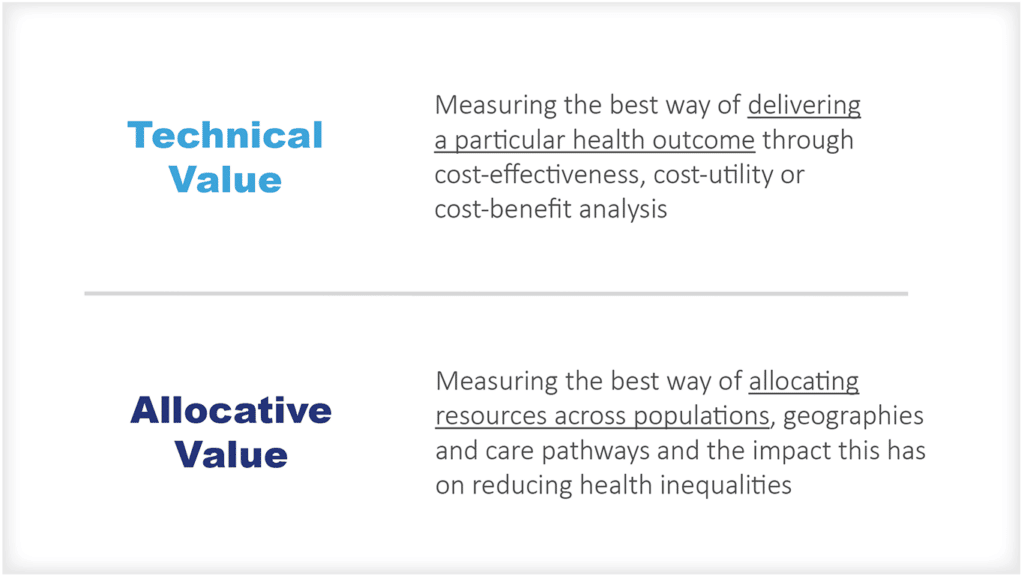
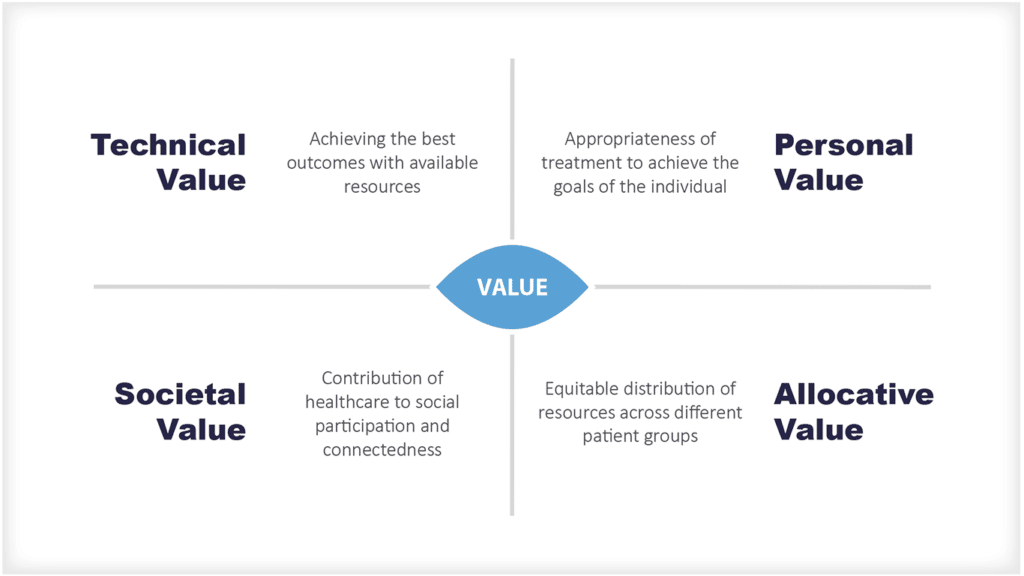
Placing health economics or monetary values on health data is extremely difficult. The health economics of health informatics are largely “intangible”. However, in 2019, a paper published by EY ‘Realising the value of health care data – a framework for the future’, proposed an approach to measuring value, which, when applied to NHS patient data suggested that the value of the NHS (England) curated data set could be as much as £5bn per annum, plus an addition of £4.6bn per annum in benefits to patients.
These estimates combined operational efficiency savings, improved patient outcomes, and wider economic impacts relating to the use of real-world data, AI and personalised medicine.
Useful References
WHO, Health System Performance Assessment, Health Policy Series 57, 2022 (ed. Irene Papanicolas, Dheepa Rajan, Marina Karanikolos, Agnes Soucat, Josep Figueras.)
Caitlin Main, Madeleine Haig, Panos Kanavos “The Promise of Population Health Management in England: From Theory to Implementation” October 2022. LSE Health and Social Care Working Paper No. 34
OECD (2022), Health Data Governance for the Digital Age: Implementing the OECD Recommendation on Health Data Governance, OECD Publishing, Paris,https://doi.org/10.1787/68b60796-en.