Value of Prevention
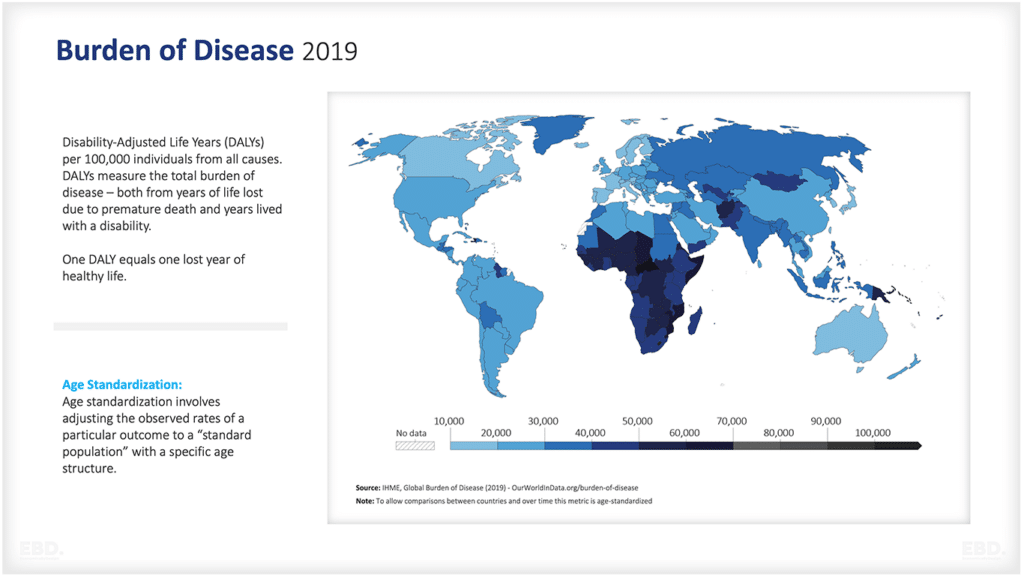
For a long time, prevention has been recognised as an important aspect of public health. It is often said that ‘prevention is better than cure’, and this applies to both physical and mental health. However, the value of prevention goes beyond just reducing the burden on healthcare systems.
Prevention can have a positive impact on the economy, as it can reduce healthcare costs and increase productivity by keeping individuals healthy and able to work. So not only does prevention benefit individuals, but it also has wider societal and economic benefits.
The value of prevention in public health is closely linked to the determinants of health and health inequalities. By promoting healthy behaviours and addressing social, economic, and environmental factors that impact health, prevention can help reduce health inequalities and promote equity in communities.
So, it is important for governments, healthcare systems, and individuals to prioritise prevention as a key component in improving overall public health. Prevention is a wise investment that brings both short-term and long-term benefits to individuals, communities and societies as a whole.
This economic lens will explore the value of prevention in more detail, looking at its impact on individuals, communities and economies. It will also discuss some successful prevention strategies and their potential for improving public health outcomes.
What Are The Main Determinants of Health?
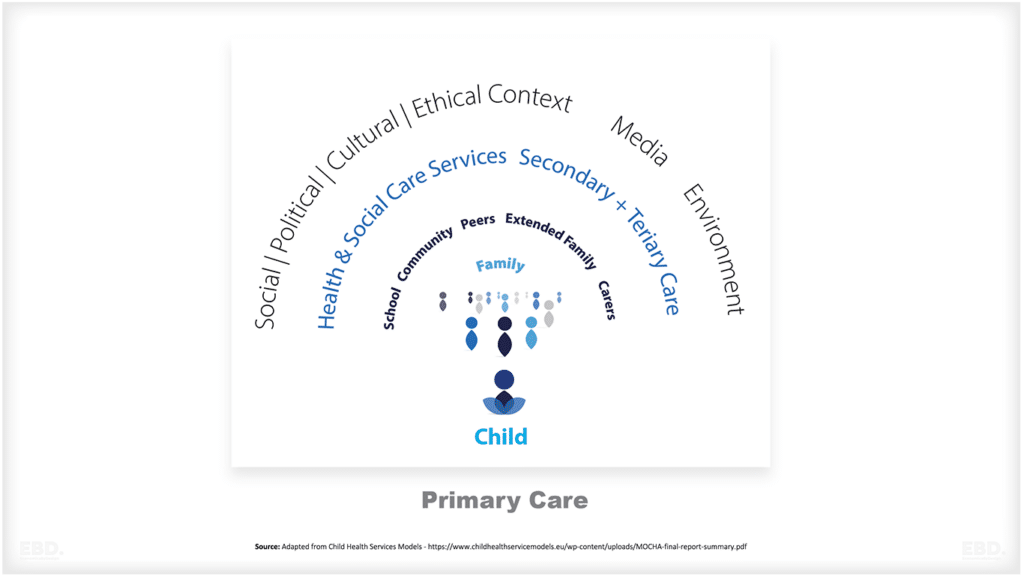
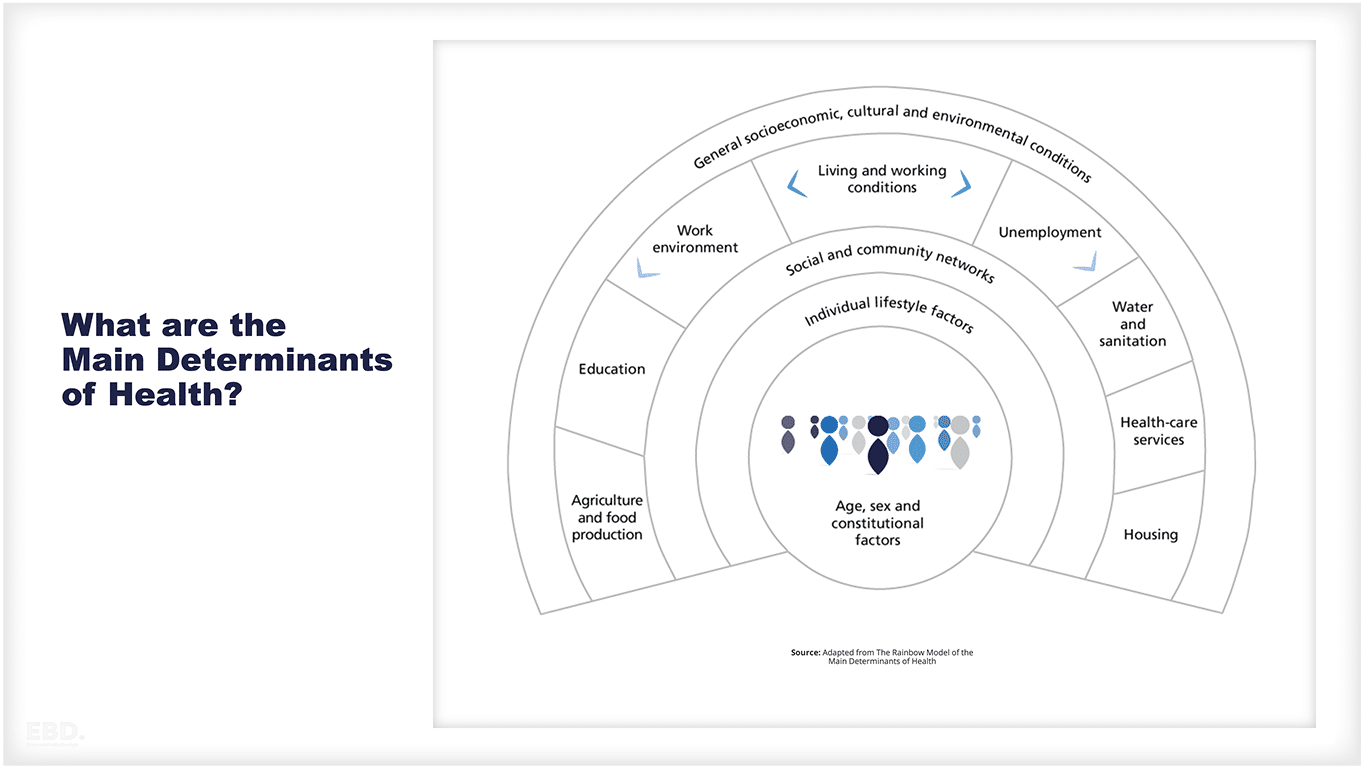
Determinants of health encompass a multitude of factors that impact an individual’s well-being. These factors span a wide spectrum, including social, economic, and environmental elements. These determinants can either positively or negatively affect an individual’s health and can have long-term impacts on their overall quality of life.
The Rainbow model of the main determinants of health, as proposed by Dahlgren and Whitehead (1991), offers a valuable framework for comprehending the intricate interplay among different factors that contribute to an individual’s health. This model portrays a diverse array of determinants, ranging from personal choices and lifestyle to social networks, living and working conditions, and wider socio-economic, cultural, and environmental contexts. It emphasises the dynamic nature of health and recognises that it is not just a product of individual behaviour or genetics, but also influenced by external factors.
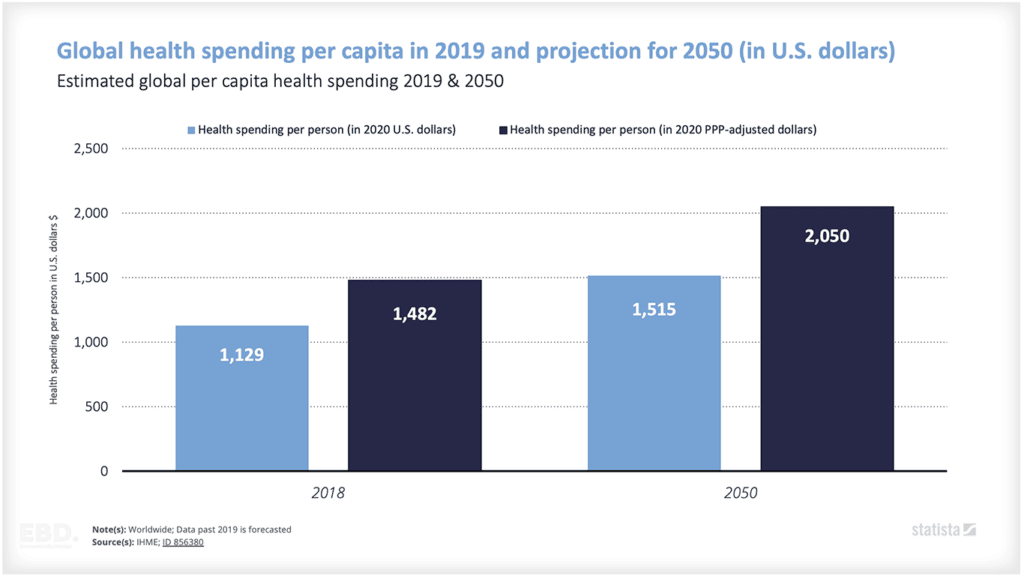
There have been many quoted estimates of the relative contribution of different determinants of health – the most comprehensive synthesis is presented here along with estimates of US intervention spending.
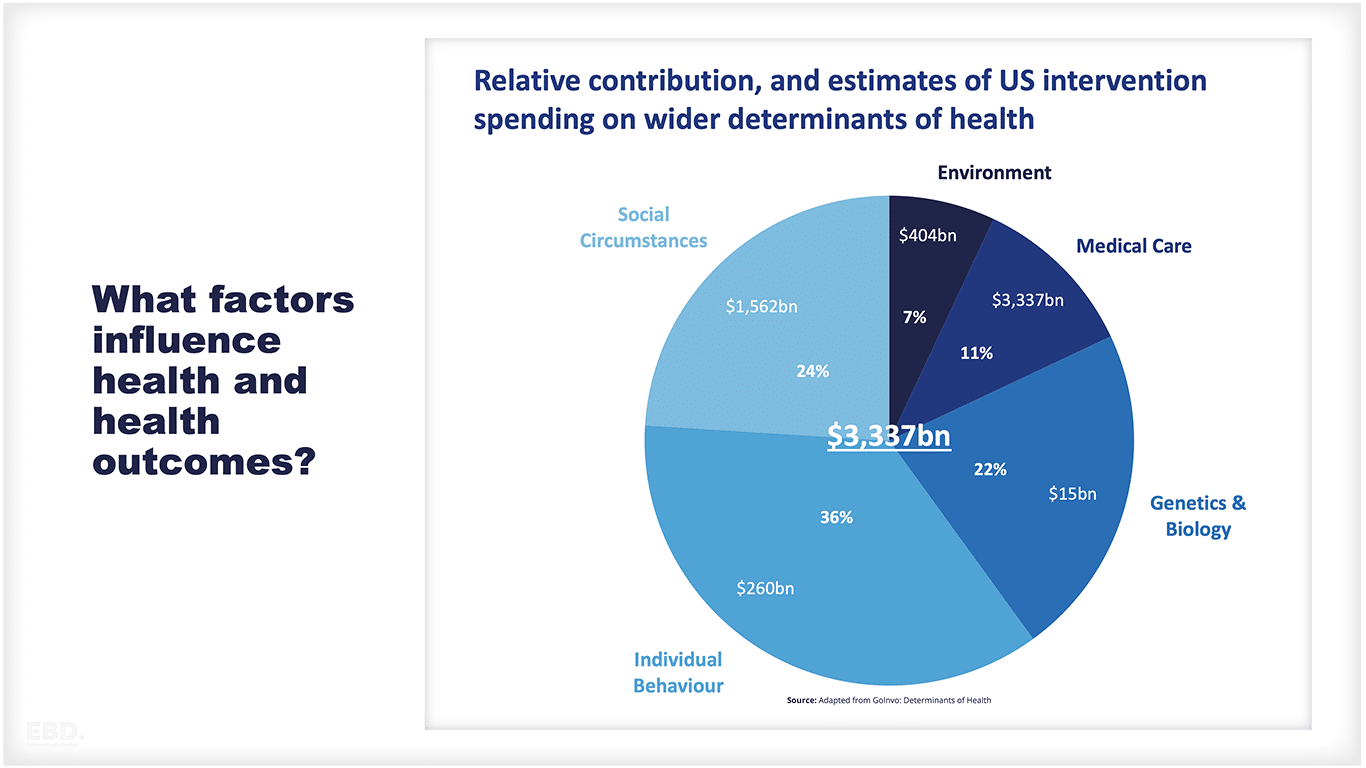
Understanding the relative contributions of these determinants and the corresponding intervention spending provides valuable insights into the complex factors that shape overall health outcomes.
As can be seen, in the US, the spending on medical care is significantly more than the combined value of spending on addressing the health impacts of wider determinants of health, despite medical care only accounting for 11% of the variation in health outcomes.
The situation is unlikely to vary significantly in any country with an established healthcare system.
What Are The Wider Determinants of Health In The United Kingdom
There has been considerable research undertaken in the UK regarding the wider determinants of health. These are the socio-economic and environmental drivers that affect people’s health, risk of disease, and likelihood of recovery. The main examples are listed below with links to further resources;
Built and Natural Environment – The quality of the environment can have a significant impact on an individual’s health, from access to green spaces for physical activity to exposure to air pollution.
Work and the Labour Market – Employment status, working conditions, and job insecurity can all affect an individual’s health. Job loss or unemployment can also have a profound impact on an individual’s well-being.
Education – Education is linked to better health outcomes as it provides individuals with knowledge and skills that can improve their overall quality of life.
Social Capital – Social networks and support systems play a crucial role in an individual’s health. Strong social networks can provide emotional, practical, and financial support during times of need.
Income – Income and socio-economic status are closely linked to health outcomes. Lower income and social position can lead to higher levels of stress, financial strain, and limited access to resources that promote good health.
Crime – Living in areas with high crime rates can contribute to feelings of insecurity and stress, which can have a negative impact on an individual’s health.
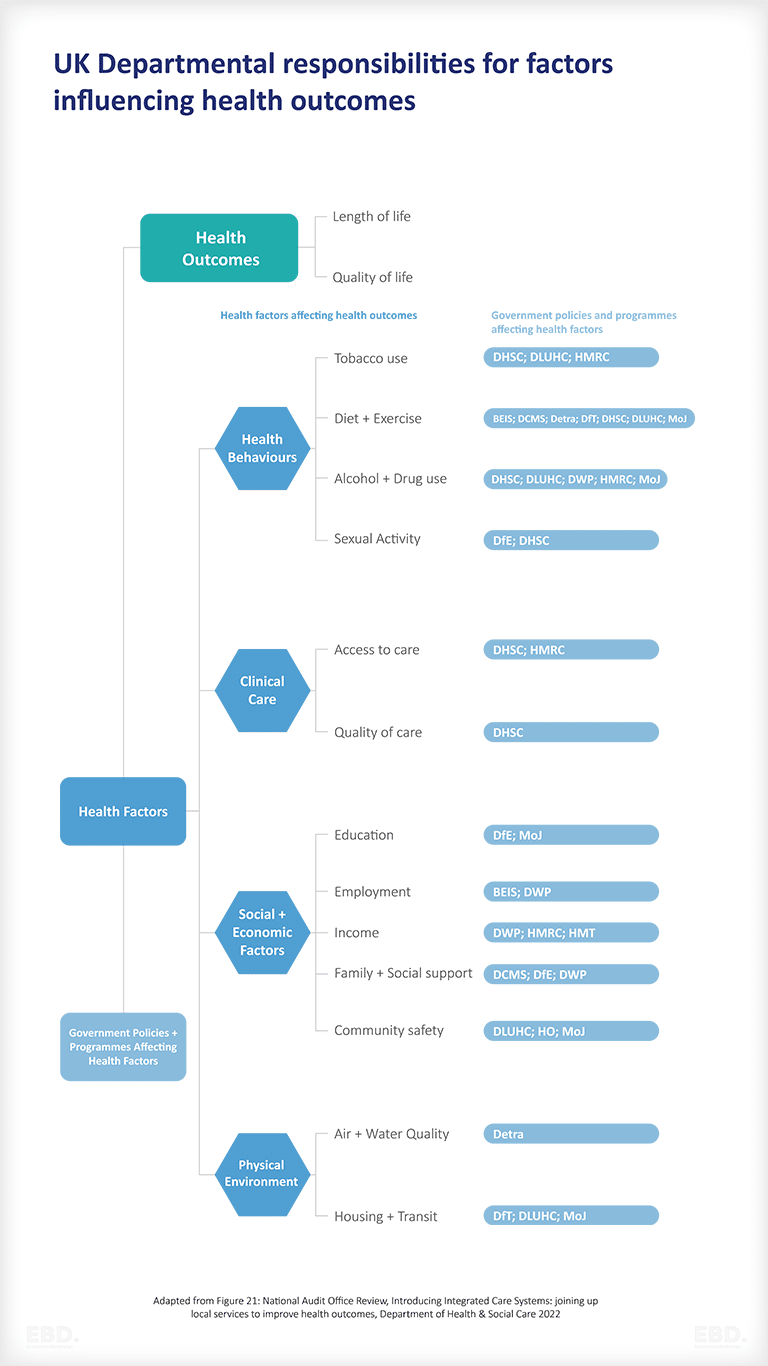
Wider determinants of health are normally the responsibility of many different public agencies and that makes coordination of actions to address health issues so difficult.
As an illustration, the diagram below depicts the allocation of national responsibilities for wider determinants across various UK government departments.
A coordinated approach at the national level involves a minimum of 12 different departments:
- Department of Health and Social Care
- Department of Local Urban Health and Communities
- Her Majesty’s Revenue and Customs
- Department for Business
- Energy and Industrial Strategy
- Department for Digital, Culture, Media & Sport
- Department of Transport
- Ministry of Justice
- Department of Education
- Department of Work and Pensions
- Home Office, Department for Environment, Food & Rural Affairs
What Are Health Inequalities?
Health inequalities refer to disparities in health outcomes, access to care, and health determinants among different population groups, primarily due to social or economic disparities. According to NHS England, these inequalities are characterised as “unfair and avoidable differences in health across the population, as well as within different societal groups.” Measurement of health inequalities often involves examining variations in life expectancy, outcomes for specific diseases or health conditions, and access to healthcare services.
It is estimated that nearly half of the variations in health outcomes are explained by unequal distribution of social and environmental factors. The institute of health equity has many studies to back this up and the Office for Health Improvement and Disparities has published a Wider Determinants of Health tool to help local authorities benchmark themselves on a range of indicators.
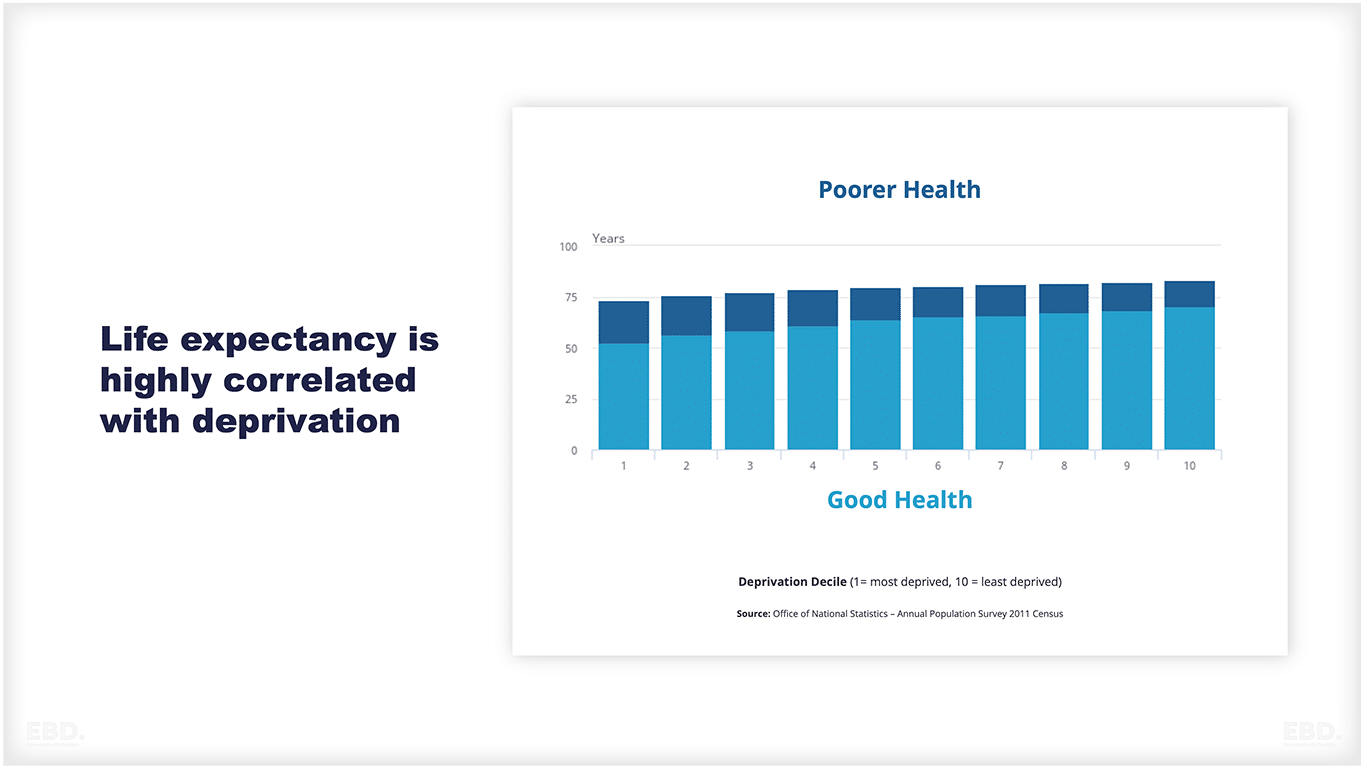
For instance, there is a strong correlation between deprivation and the variation in life expectancy. A recent publication by the Tony Blair Institute reveals a remarkable 27-year gap in male life expectancy between the London borough of Kensington and Chelsea and Blackpool. In Kensington and Chelsea, men can now expect to live up to 95.3 years, while in Blackpool, the figure is a mere 68.3 years. This stark contrast highlights the significant disparity in life expectancy across different regions in England. Furthermore, the figure below demonstrates that males residing in more deprived areas are expected to live less than three-quarters of their lives in good health.
Reducing Health Inequalities
One way of reducing health inequalities, could be to focus on prevention interventions that tackle the underlying social determinants and environmental factors. This includes actions such as improving living conditions, increasing access to education and employment opportunities, promoting healthy behaviours, and reducing exposure to risks like pollution and crime.
If left unaddressed health inequalities are expensive; in the UK, a study published in 2014 by the Institute of Health Equity, from Frontier Economics, estimated that health inequalities in England resulted in:
- Economic losses of between £31 and £33 billion based on the value of lost productivity associated with lost working days
- £5.5 billion in costs to the NHS
- A fiscal impact (lost taxes and higher welfare payments) of between £20 and £32 billion.
Another study of the economic cost of health inequality across Europe (Mackenbach et al, 2011), suggests that health inequalities result in a 1.4% loss to the economy (as measured by GDP) per annum.
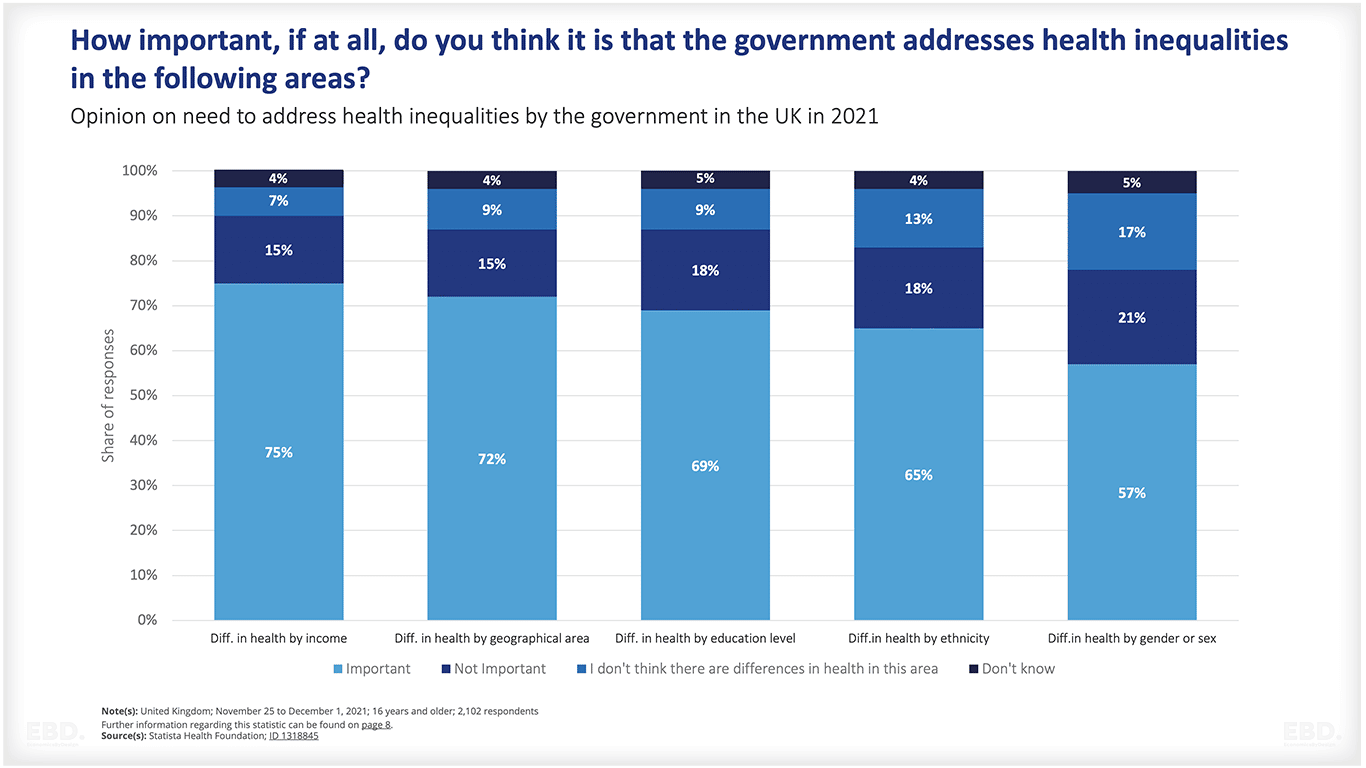
Targeting prevention on disadvantaged populations is supported by the public. A recent IPSOS survey in the UK published by the Health Foundation suggested that the general population in the UK thinks that it is important for the government to act to reduce health inequalities, particularly where it relates to differences in income and geography.
What are Prevention Interventions?
Prevention Interventions can be considered at three levels:
- Primary Prevention: refers to interventions that aim to benefit the entire population. These proactive measures are designed to decrease the occurrence of diseases and health issues by addressing lifestyle risk factors. Examples include widespread campaigns and general warnings to discourage smoking.
- Secondary Prevention: involves tailored actions based on an individual’s risk. It entails the systematic detection of early stages of diseases and intervening before full-blown symptoms emerge. An example of this is prescribing statins to lower cholesterol levels or implementing measures to reduce high blood pressure.
- Tertiary Prevention: Softening the impact of an ongoing illness or injury that has lasting effects. This is done by helping people manage long-term, often-complex health problems and injuries (e.g. chronic diseases, permanent impairments) in order to improve as much as possible their ability to function, their quality of life and their life expectancy.
Primary Prevention Interventions
Primary prevention interventions aim to prevent the onset of disease or injury by addressing factors such as lifestyle, environment and social determinants. These interventions promote healthy behaviours and reduce exposure to potential health hazards.
Examples of primary prevention measures include:
- Vaccination policies and programmes to control infectious diseases, especially in early childhood.
- Clean drinking water and sanitation.
- Traffic safety measures to prevent accidental death, including speed limits, laws requiring use of seatbelts and infant/child seats.
- Limits on tobacco use: license laws and taxes for sales, restrictions on consumption such as smoke-free environments in public places (public buildings, hospitals, schools, auditoriums, restaurants/bars), clinical support to stop smoking (especially antenatal).
- Limits on alcohol purchasing and consumption: licence laws and taxes for sales, restrictions on consumption such as designated places and times, clinical support for addiction recovery such as alcohol care teams.
Secondary Prevention Interventions
Secondary prevention interventions aim to detect and reduce the impact of diseases or injuries at an early stage. These interventions include methods for early detection, diagnosis and treatment, with efforts also made to prevent further progression of the disease.
Examples of secondary prevention measures include:
- Screening programs for various health conditions such as cancer (e.g. mammograms, colonoscopies), hypertension, diabetes, and sexually transmitted infections
- Regular health check-ups and follow-up appointments for those with existing chronic conditions
- Early intervention programs for children with developmental delays or disabilities
- Implementation of policies to reduce exposure to environmental toxins (e.g. air pollution)
Tertiary Prevention Interventions
Tertiary prevention interventions aim to improve the quality of life and functioning of individuals living with long-term, often-complex health problems. These interventions focus on rehabilitation and support to help individuals manage their conditions, prevent complications, and promote independence.
Examples of tertiary prevention measures include:
- Chronic disease management programs to help individuals monitor their conditions and adhere to treatment plans
- Rehabilitation services such as physical therapy, occupational therapy, speech therapy
- Support groups for those living with chronic conditions or disabilities
- Workplace accommodations for individuals with disabilities to promote employment and economic independence
What is the Value of Investing In Prevention?
Healthy Populations -> Healthy Economies
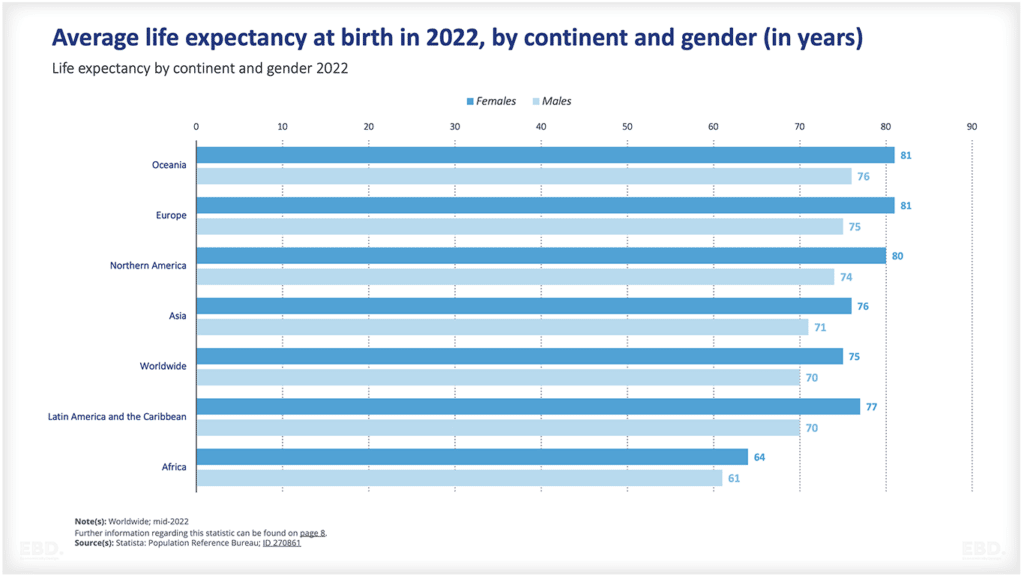
There is growing evidence of a strong causal relationship between longer healthier life expectancy and economic health. Estimates suggest, a 1 year increase in average life expectancy increases GDP per capita by 4%.
Drivers include:
- A more productive workforce.
- Lower healthcare costs, both directly and indirectly through less absenteeism.
- Increased consumer spending by older people who are living longer and healthier lives.
The Confederation of British Industry (CBI) estimates that 130 million working days are lost due to illness every year. Supporting workplace health could reduce this by between 10% and 20% to generate £60 billion annually for the UK economy – equivalent to almost 3% of GDP.
The Value of being healthy
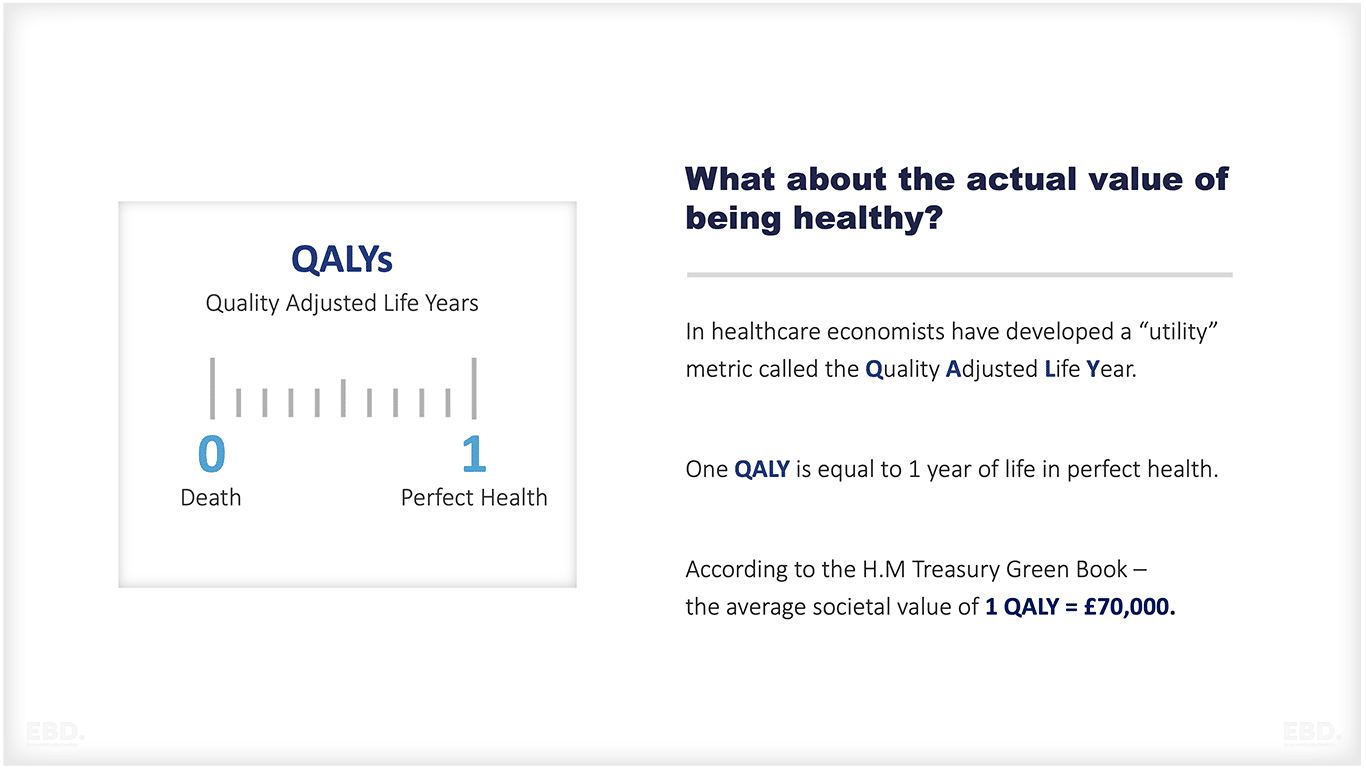
Quality Adjusted Life Years
Economists have developed a metric called Quality Adjusted Life Year (QALY). One QALY represents a year of perfect health. The Department of Health and Social Care estimates the economic value of one QALY to be £70,000. This value is based on population-based survey data known as “willingness to pay.” Many studies use this value to assess the overall value of prevention interventions.
The NICE benchmark for QALY is £20,000. This benchmark helps determine whether to allocate resources to one intervention over another. If an intervention generates more than 1 QALY for £20,000, it improves value for money. Conversely, if it generates less than 1 QALY, it reduces value for money. Independent estimates from York University support this productivity benchmark, suggesting that every £20k of NHS spending generates an additional QALY.
Considering the return on investment (£20k spent for a return of £70k), increasing the overall NHS budget seems logical, not to mention the wider economic benefits.
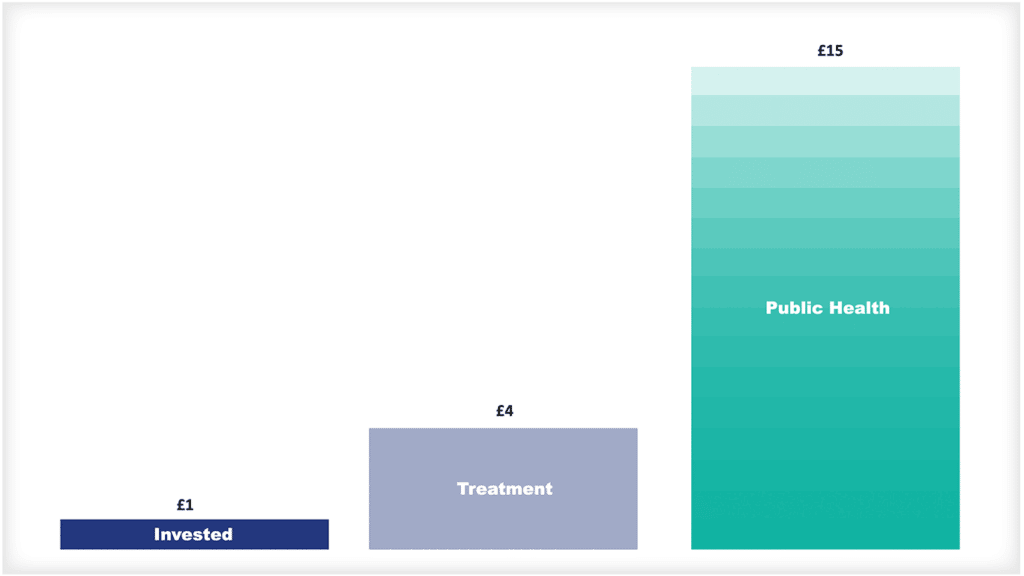
Investing in Prevention
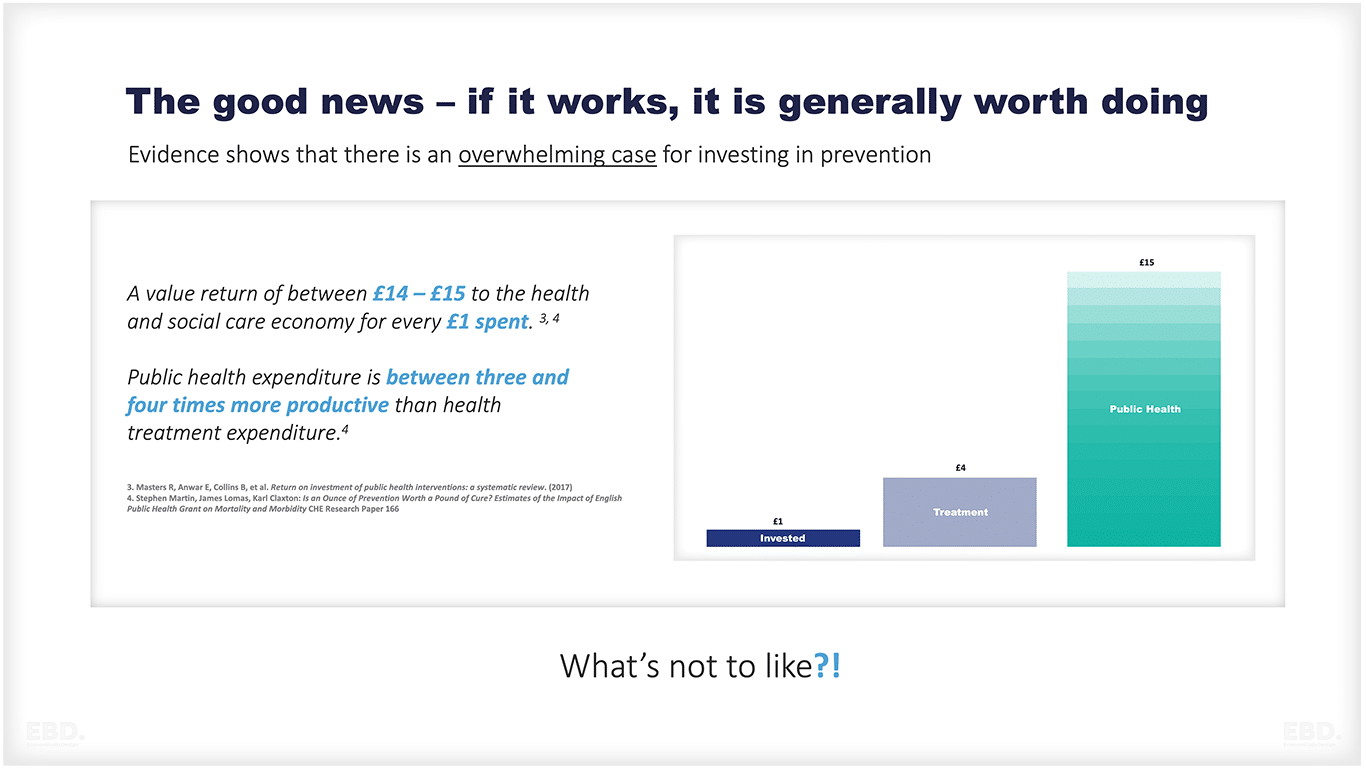
Furthermore, studies suggest that every £1 spent on preventative healthcare generates a £14 – £15 return to the health and social care economy and that public health expenditure is between three and four times more productive than health treatment expenditure.
Case Studies and Return of Investment Tools
The Office for Health Improvements and Disparities has an abundance of evidence of cost effective prevention interventions from Public Health England and NICE. The repository of evidence shows over 370 interventions covering all of the major primary interventions and some secondary interventions.
Public Health England’s Health Economics and Modelling Team (HEMT) provides resources to estimate the value of investing in prevention and early diagnosis. These resources consolidate evidence on costs, savings, and health benefits, simplifying commissioning of cost-effective services. This includes Return On Investment tools to estimate the impact of interventions on costs and health outcomes in local authorities and CCGs. Examples of ROI studies and tools targeting particular behaviours or care pathways are listed below;
- Best Start in Life
- cardiovascular disease
- contraceptive services(and an extension to the contraception ROI tool)
- falls prevention
- mental health services
- musculoskeletal conditions
- oral health in pre-school children
- older adults
- sexual and reproductive health in young people
- weight management
- colorectal cancer ROI tool
- end of life care economic tool
- NHS Diabetes Prevention Programme ROI tool
Additionally, the Health Economics Evidence Resources (HEER) tool collects and summaries economic evidence on a wide range of public health interventions. This resource enables filtering and selection using more than 20 different criteria, facilitating a targeted approach to areas of interest.
These tools and resources are just a few examples of the numerous return on investment tools available for assessing the economic value of prevention interventions. By utilizing these tools, health and social care organizations can make informed decisions about resource allocation, maximizing the benefits and cost-effectiveness of their investments in preventative measures. With an increasing focus on preventative healthcare and evidence-based decision making, these return on investment tools play a crucial role in shaping the future of healthcare. So, it is essential to continue developing and using these valuable resources to optimize health outcomes and reduce healthcare costs for individuals and society as a whole.
What are the barriers to realising value from Prevention?
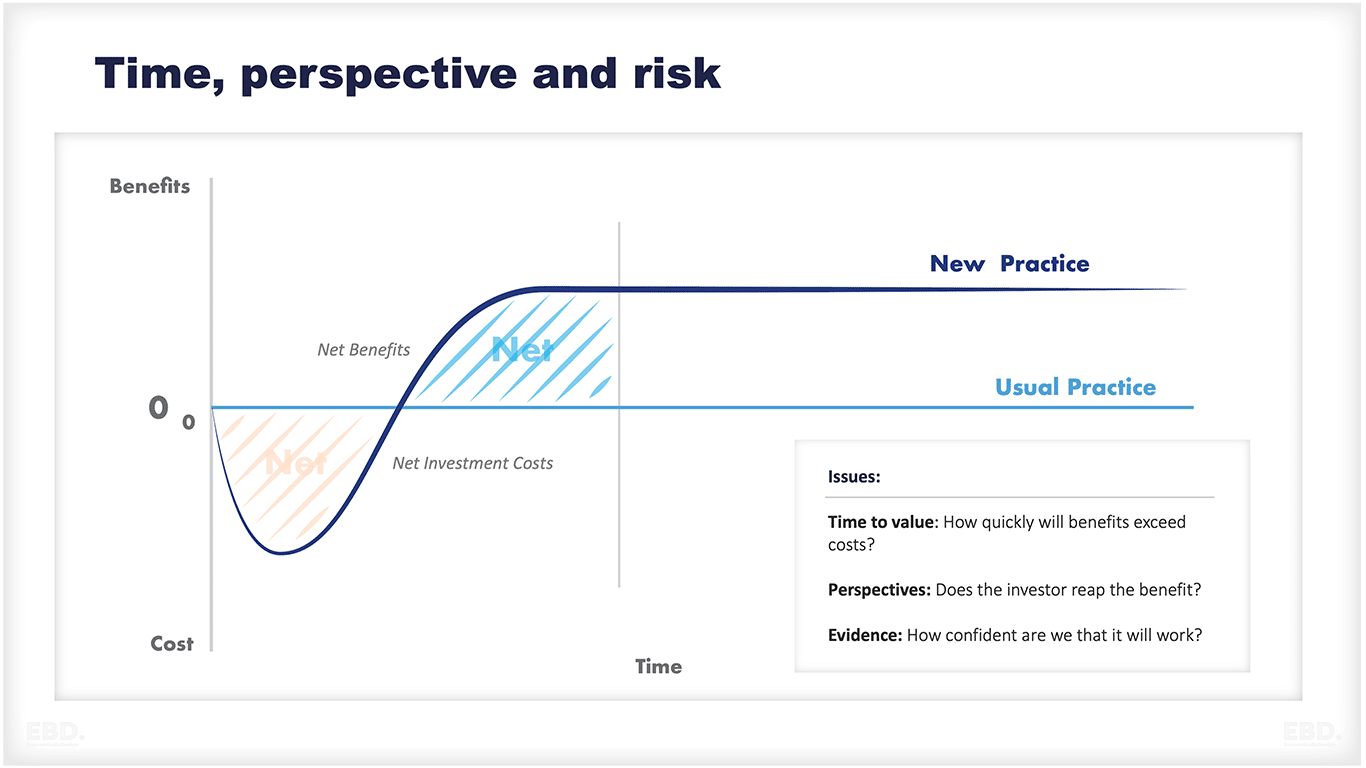
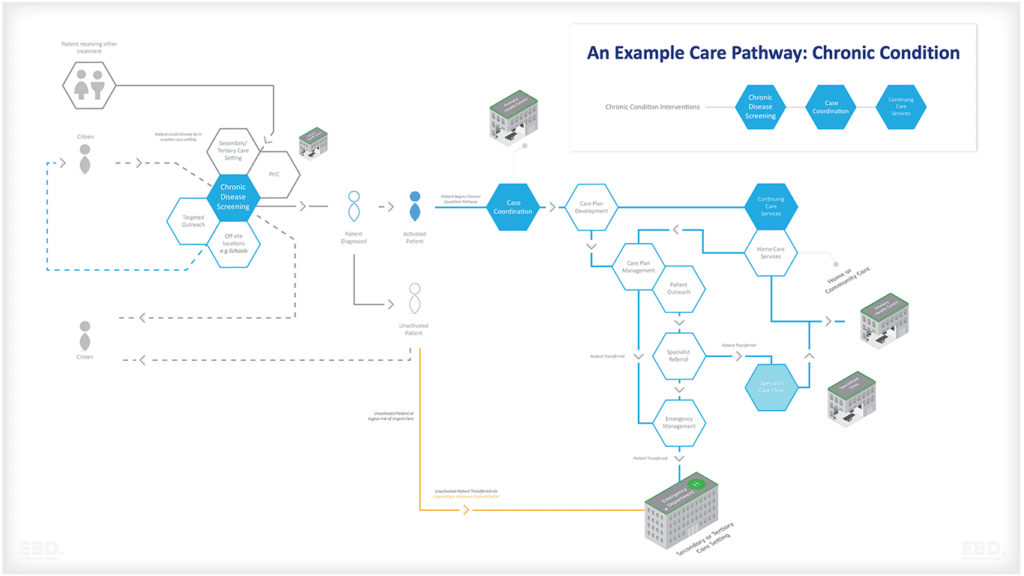
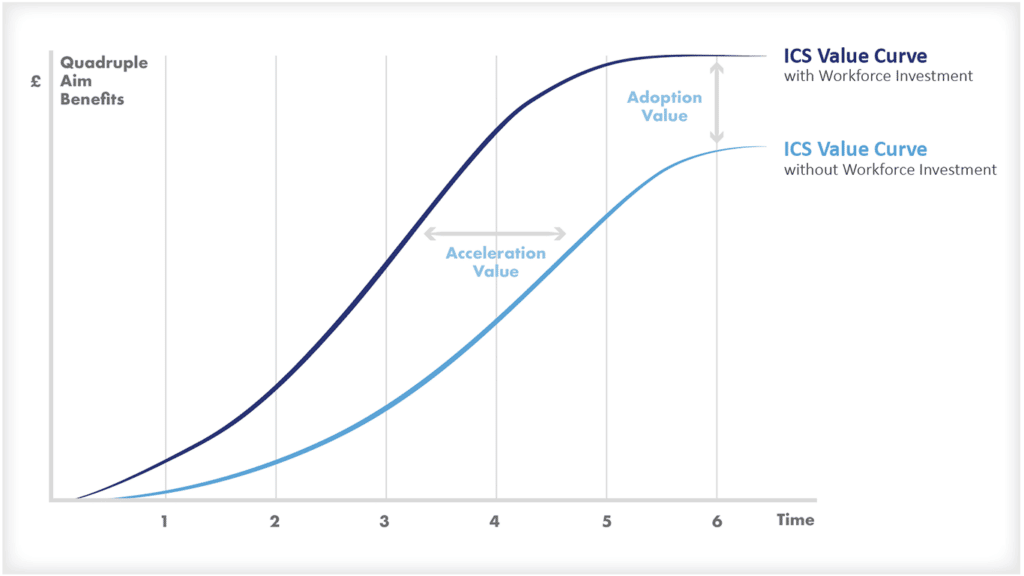
Although prevention interventions have clear benefits and potential cost savings, as shown in the figure below, their realization is hindered by several barriers.
These barriers include factors such as limited time, different perspectives, and perceived risks.
- Time to value: The benefits of preventative measures are not always immediately visible, and it can take time to see the impact. As a result, investing in prevention may require a long-term commitment, which can be challenging for health and social care organizations facing budget constraints. For example; the impact of smoking cessation on reducing deaths from lung cancer can take years – especially when it relates to stopping young people from ever smoking.
- Perspectives: It is difficult to rely on local provider organisations to reorientate care from treatment to prevention unless funding flows and payment models reward these activities.
- Perceived risk: is another barrier that may prevent organisations from investing in prevention. There may be hesitancy towards implementing unproven or new interventions, especially when there are existing treatments available. This is where evidence-based decision making becomes critical in demonstrating the value and effectiveness of preventative measures.
However, the perception of risk and lack of immediate impact can make it challenging to reallocate funds from treatment to prevention. It is important for organisations to carefully assess and plan how they will integrate prevention into their practices without sacrificing the quality and accessibility of current treatments. By utilising return on investment tools and evidence-based decision making, organisations can make informed decisions about resource allocation that prioritise.
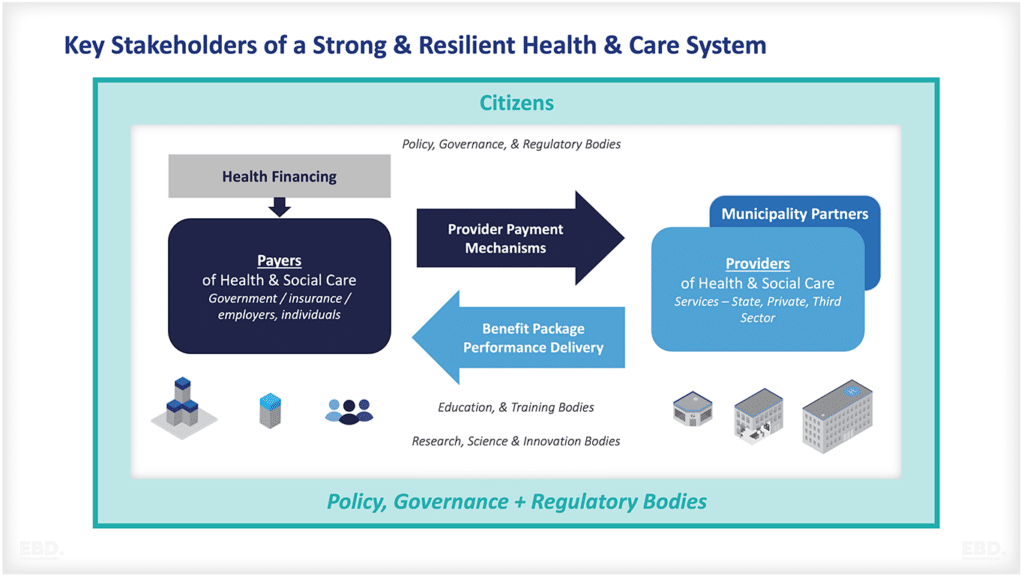
What role should an Integrated Care System play?
Integrated Care Systems provide real opportunities for increasing investment in prevention.
The NHS in England has recently introduced 42 Integrated Care Systems each of which has 4 overall aims:
- Improve outcomes in population health and healthcare
- Tackle inequalities in outcomes, experience and access
- Enhance productivity and value for money
- Help the NHS support broader social and economic development
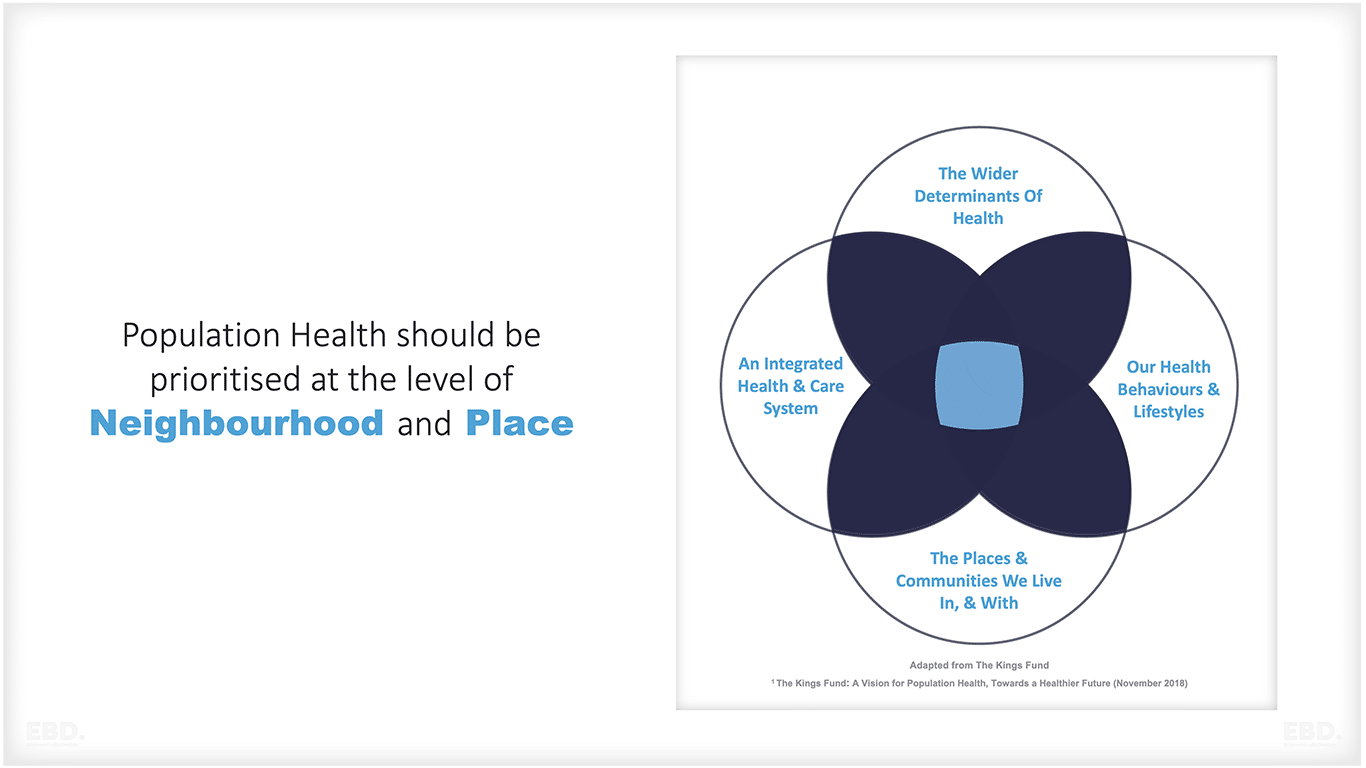
Each Integrated Care System will collaborate on setting local goals and targets for the geographies and organisations within the scope of their governance. This will include shared goals and targets for “place” and within these “neighbourhoods”. It will include goals for public health, health service delivery and social care.
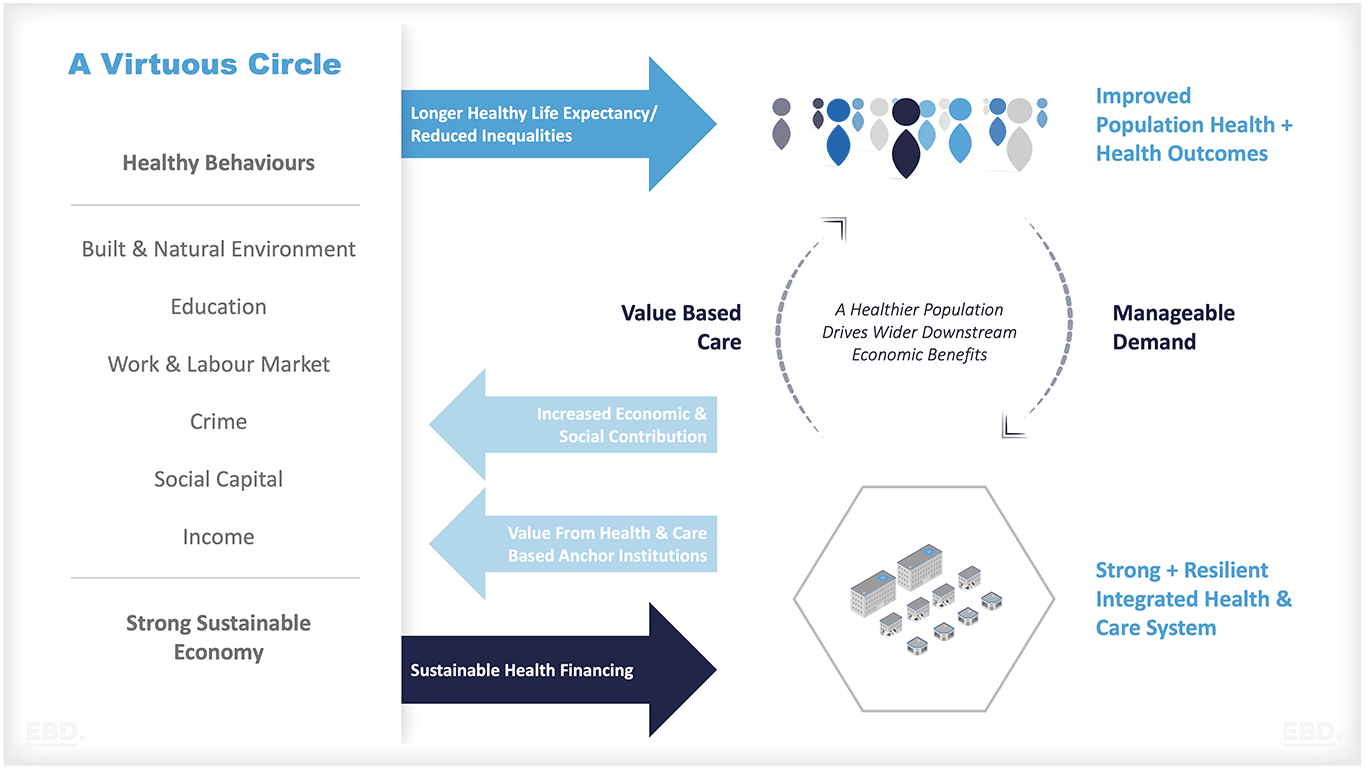
The goal is to create a positive cycle, focusing on wider determinants of health, such as the built and natural environment, education, work, crime, social capital, and income.
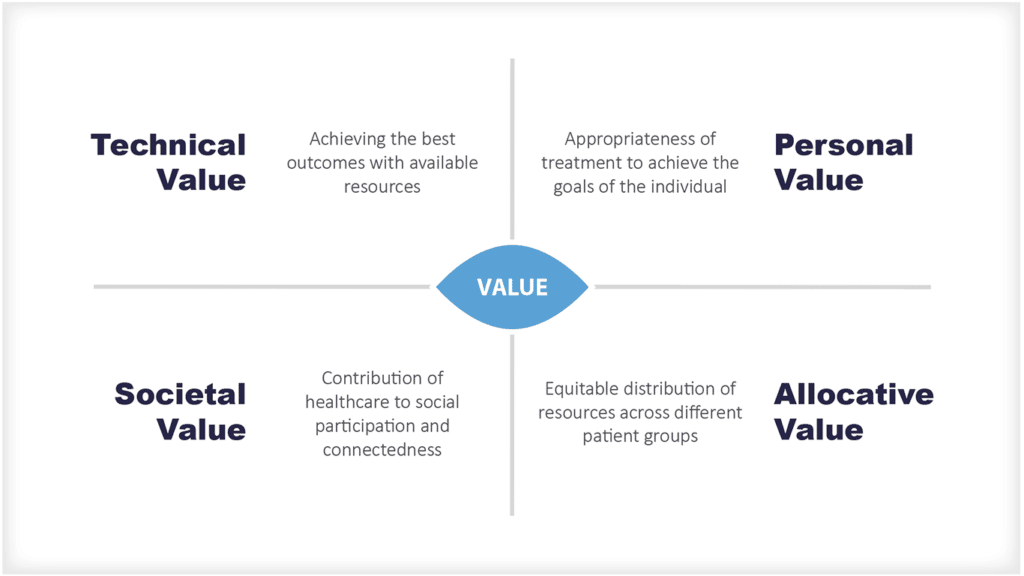
This approach aims to promote longer and healthier lives, reduce health disparities, and enhance overall population health. By delivering value-based care through an Integrated Care System (ICS), population health, wellness, prevention, and efficient treatment coordination can be prioritised.
The ICS, as an anchor institution, plays a significant role in influencing development and serves as a local employer and pillar of the community, contributing to economic and social growth while supporting sustainable health financing. This cycle is summarised in the diagrams below.
The concept revolves around the ability of the ICS to prioritize the health of the population, specifically at the neighborhood and local level. This entails empowering the ICS with the authority to make informed decisions that benefit the well-being of communities.
The ICS is supposed to to develop and target interventions at the CORE20PLUS5; the core most deprived 20% of the national population, PLUS population groups at a local level with particular needs, and groups with protected characteristics across 5 clinical areas, namely maternity, severe mental illness, chronic respiratory disease, early cancer diagnosis and hypertension. Local areas are being encouraged to use this framework to develop initiatives targeted to improve health outcomes for these populations, and hence reduce health inequalities.
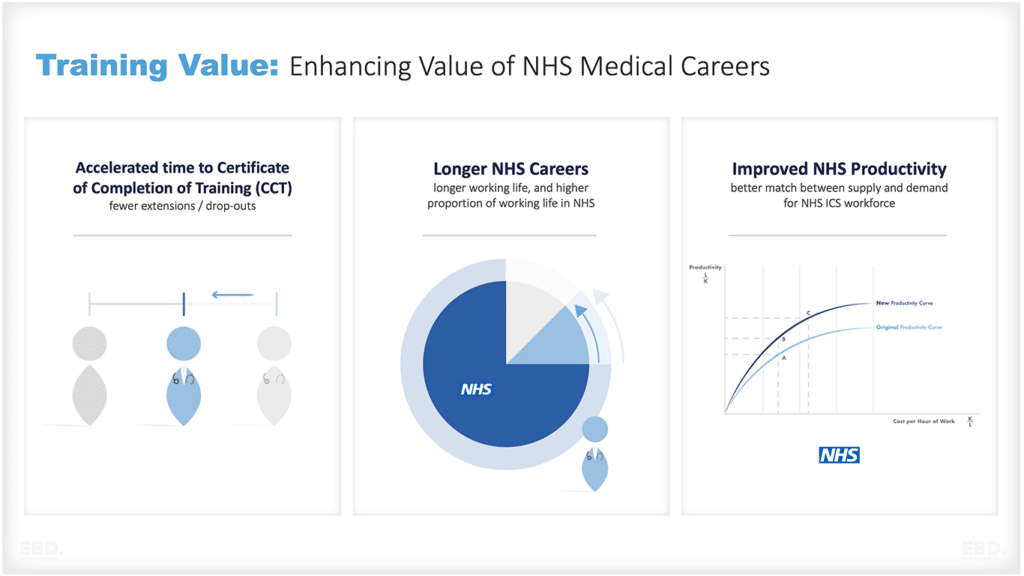
Unless there is alignment of funds at the top, specifically in terms of budgets for prevention, social care, and wider determinants, Integrated Care Systems (ICSs) will face significant challenges. However, ICSs possess substantial resources that can be leveraged to overcome barriers that previously hindered providers from reallocating their existing resources. This includes reevaluating workforce roles and job descriptions, as envisioned by the “Enhance” programme, as well as reorienting care models to enable system-wide collaboration in designing and delivering care pathways.
Using smoking as an example, NICE has recently updated its guidelines which includes many recommendations about the role of schools, smoking cessation services, support in secondary care settings and support for pregnant women. The idea is that the ICS will have a system-wide smoking prevention strategy which is a watermark through all of its contracts. An example of this type of prevention in action is the West Suffolk smokefree maternity pathway to support healthy pregnancies. This should have short term returns particularly in relation to low birth weight babies.
One final note of caution; it is very tempting for an ICB (rather than the ICS) to drive todays prevention priorities solely towards addressing todays acute hospital pressures e.g. preventing repeat admissions, preventing falls, preventing frailty admissions, but this too can result in missed opportunities for small cultural shifts that can reduce harmful behaviours in the longer term – and the associated disease burden.
Conclusion
Prevention must be a priority for organisations in the healthcare sector. By utilising evidence-based decision making and prioritising resource allocation through return on investment tools, preventative measures can be integrated into existing practices without sacrificing the quality of current treatments. Integrated Care Systems play a crucial role in this process by aiming to improve outcomes and tackle inequalities through collaboration, setting local goals and targets, and focusing on the wider determinants of health.