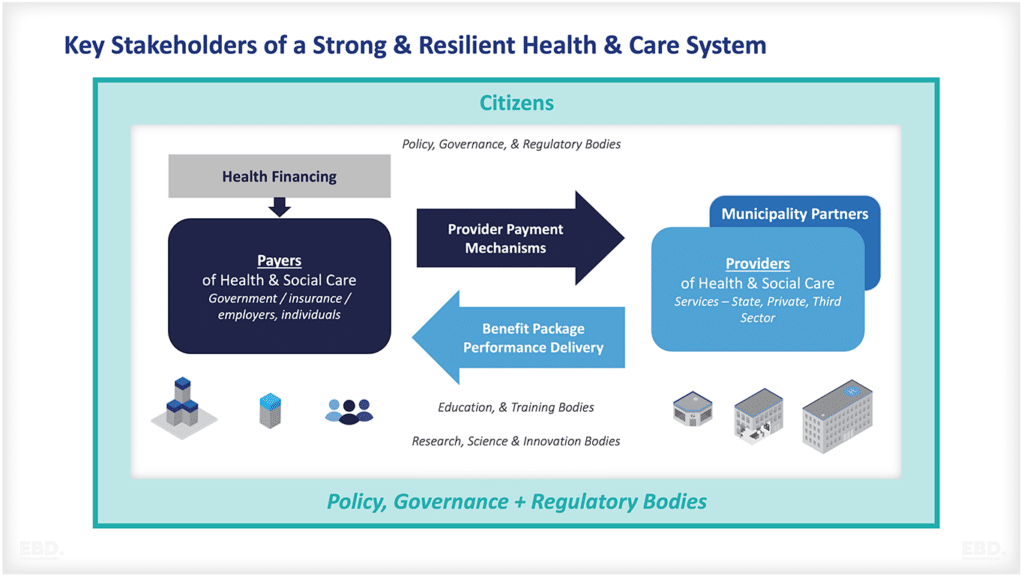
Health Financing
Health financing is a critical enabler of Universal Health Coverage (UHC). It ensures that people can access the universal coverage for health services they need without suffering financial hardship.
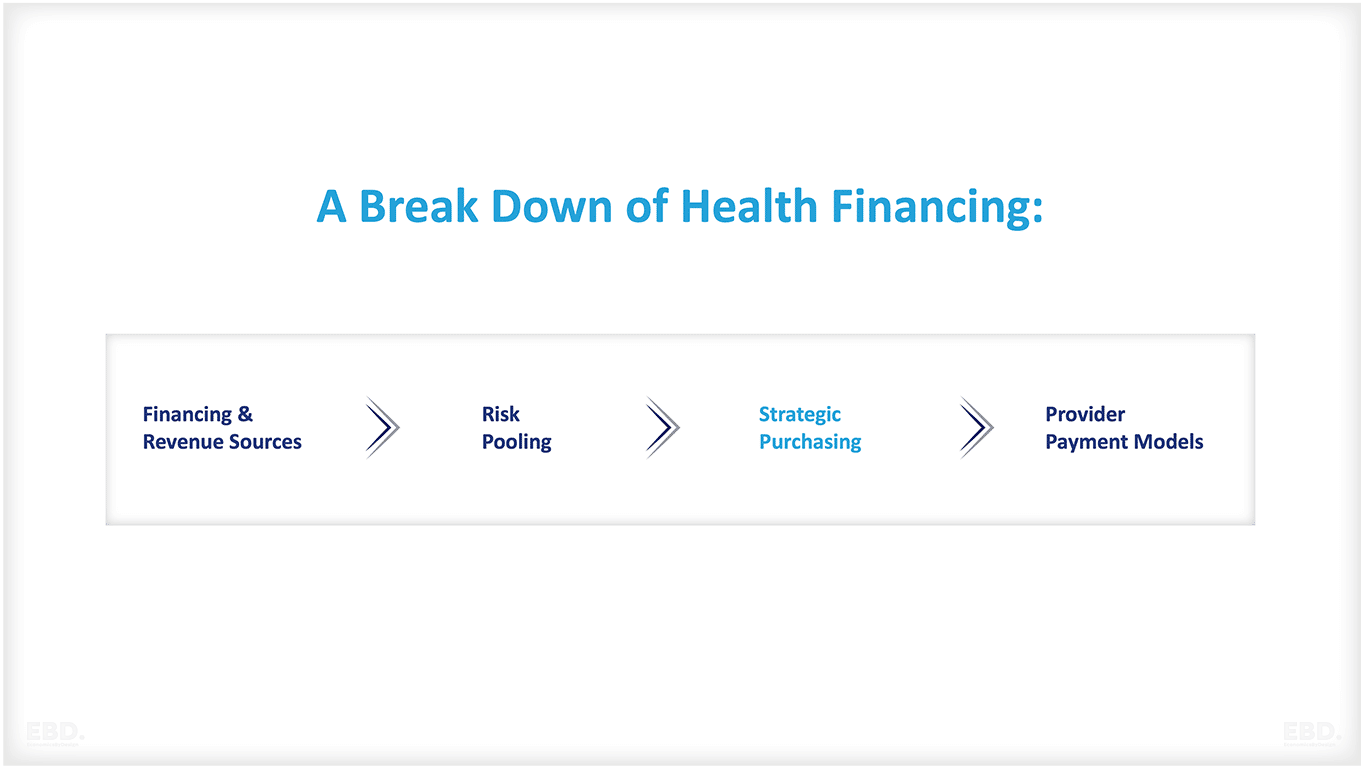
There are many different ways to flow funds through the health care system, but all systems have four basic elements:
Financing & Revenue Sources
This is when funds are gathered from people to pay for health care needs. This can be done at scale through government contributions, taxes, social insurance contributions, private insurance contributions, or philanthropic contributions. It also includes out-of-pocket payments by individuals paying directly for treatment when it is needed.
Risk Pooling
Funds gathered at scale can be pooled together in a way that allows them to be used more efficiently and effectively. This means that the risks of needing healthcare are shared among a larger group of people, which helps to keep costs down. Pooling can be done through a single fund for a whole health system, regional funds for sub-national systems, or multiple funds for specific population groups.
Strategic Purchasing
Pooled funds are used to purchase health care services for a group. This can be done directly by the government or through private insurers. It includes making contracts with providers, setting prices, and ensuring that quality standards are met.
Provider Payment Models
Providers (such as hospitals and doctors) need to be paid for the health care services they provide. This can be done through a variety of models, capitation, block funding, line-item funding, fee-for-service, case-based payments, or a mix of some or all. It can include incentives to improve performance or conditional on achieving pre-agreed outcomes.
The focus of this economics lens is on strategic purchasing and procurement.
What is Strategic Purchasing?
“Purchasing is a core health financing function that refers to the allocation of pooled funds to public and private health care providers for the health services they provide.“ WHO, 2019
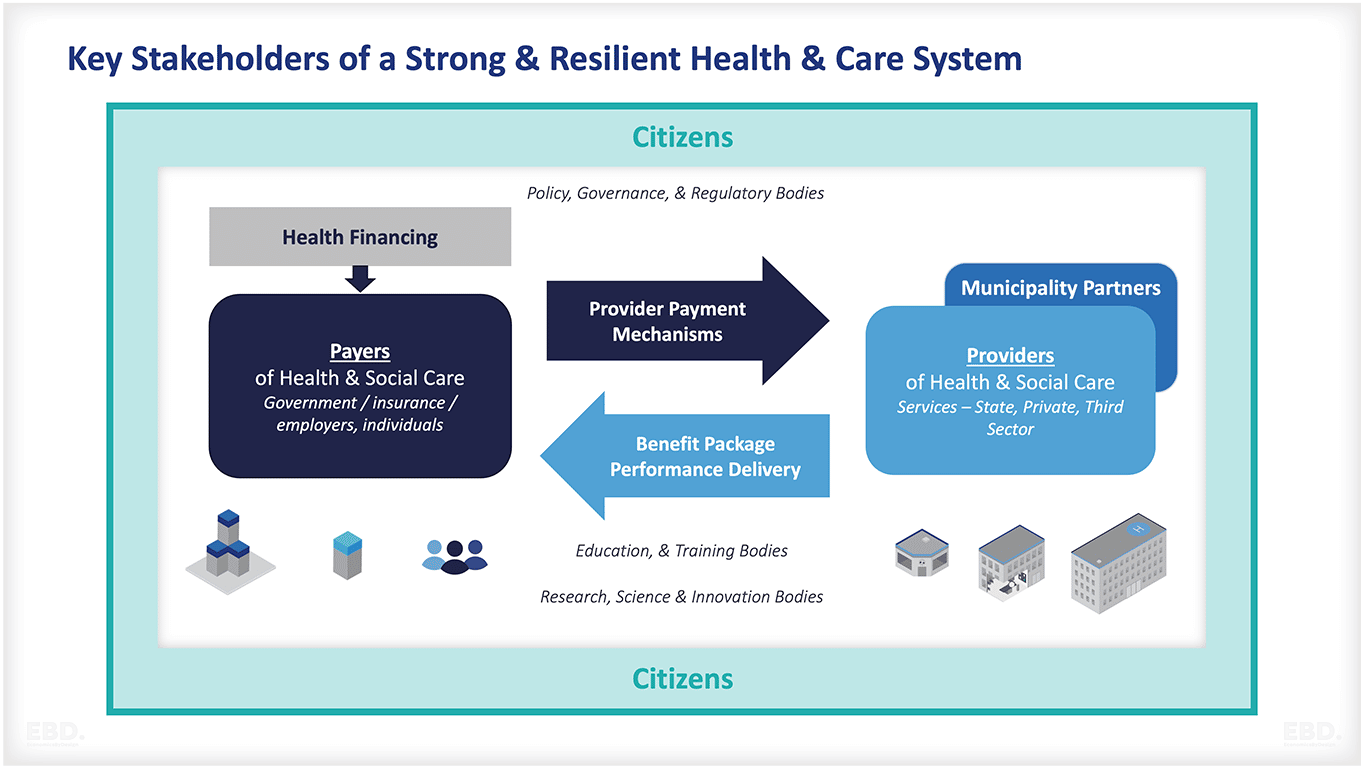
Purchasing is a key function in achieving Universal Health Coverage (UHC). It is the link between the revenue raised from financing the health system, the pooling of these funds, and the flow of funds to providers using different payment mechanisms in exchange for the delivery of services.
Purchasing involves making decisions about what services to purchase (health benefits), what (and how) to pay for them, which providers to contract with, and what quality and outcomes can be expected.
Traditionally, purchasing health services is largely transactional, with government agencies, insurance organisations and others responsible for buying services for a population group being focused on cost control whilst protecting quality.
Purchasing for UHC requires a shift in thinking; rather than focusing solely on cost, the emphasis is on achieving value in relation to a wider set of health system goals.
Health System Goals
Each country will have its own health system goals, which will be informed by its own specific context, priorities and needs. However, some broad goals are common to most health systems:
- Improving population health outcomes
- Reducing disparities in health outcomes
- Enhancing patient/consumer experience
- Improving provider/clinician experience
In recent years there has been international adoption of the triple aim and quadruple aim goals:
Triple aim
The triple aim is a framework developed by Berwick et al. (2008) and adopted by the Institute for Healthcare Improvement in the United States that aims to improve the health of a population, enhance the patient experience of care (including quality and satisfaction), and reduce per capita costs of health care.
Quadruple aim
The quadruple aim is a similar framework to the triple aim and aims to improve the patient experience of care, improve the health of populations, reduce the per capita cost of healthcare, and improve provider experience and satisfaction.
Value-Based Purchasing
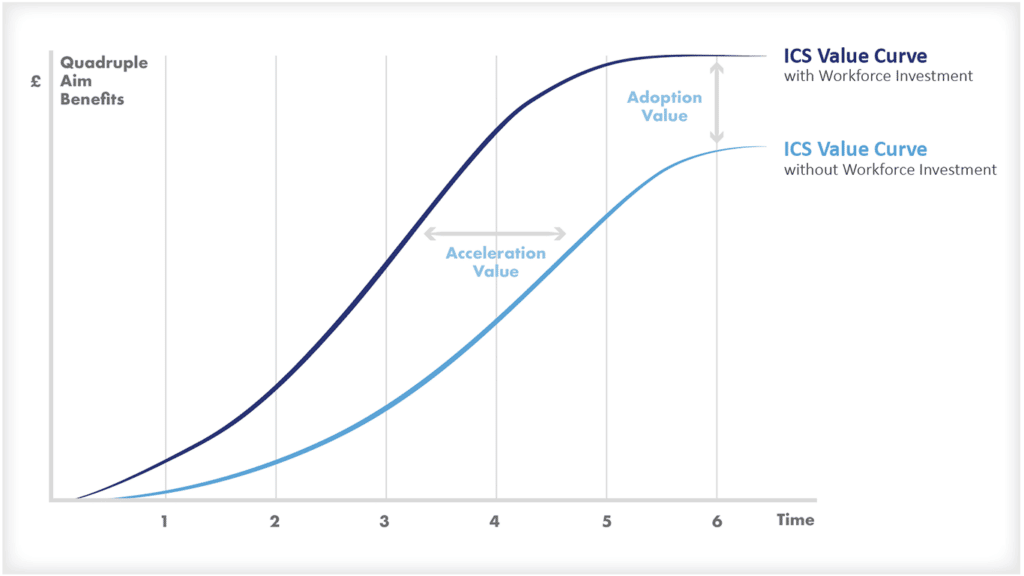
Value-based purchasing (VBP) is an approach to purchasing health services that take into account the clinical and non-clinical outcomes achieved, as well as the cost of producing those outcomes.
In other words, it is a way of looking at how much ‘value’ a healthcare intervention provides about its cost. It is sometimes also known as ‘value-based healthcare’, ‘value-based insurance design’ or ‘outcomes-based purchasing’.
The key components of VBP are:
- Defining and measuring outcomes that matter to patients, families and communities;
- Rewarding providers for achieving results rather than simply for the services they deliver;
- Encouraging providers to work together to improve care coordination and continuity;
- Making better use of information to support decision-making.
Value-Based Healthcare
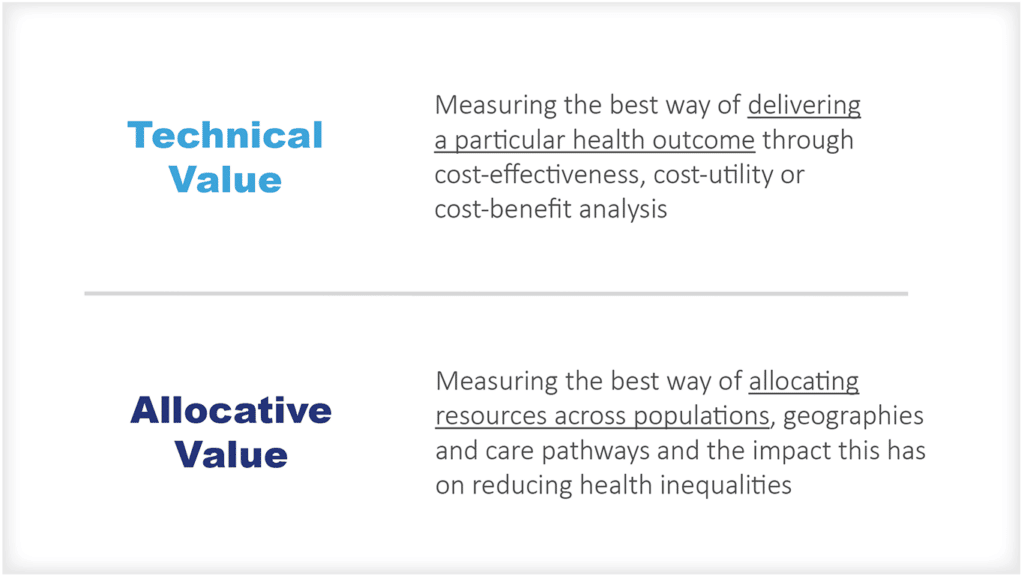
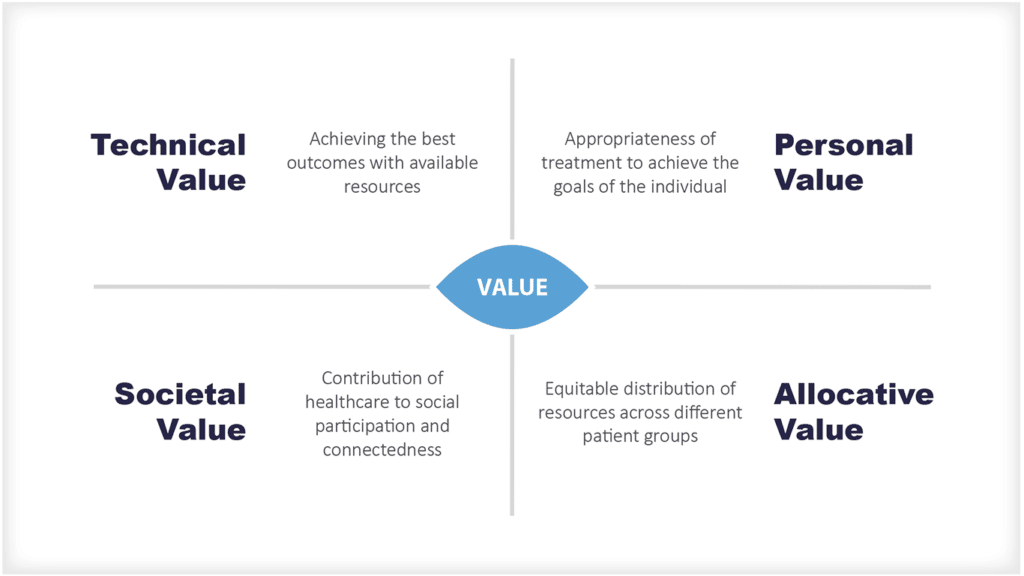
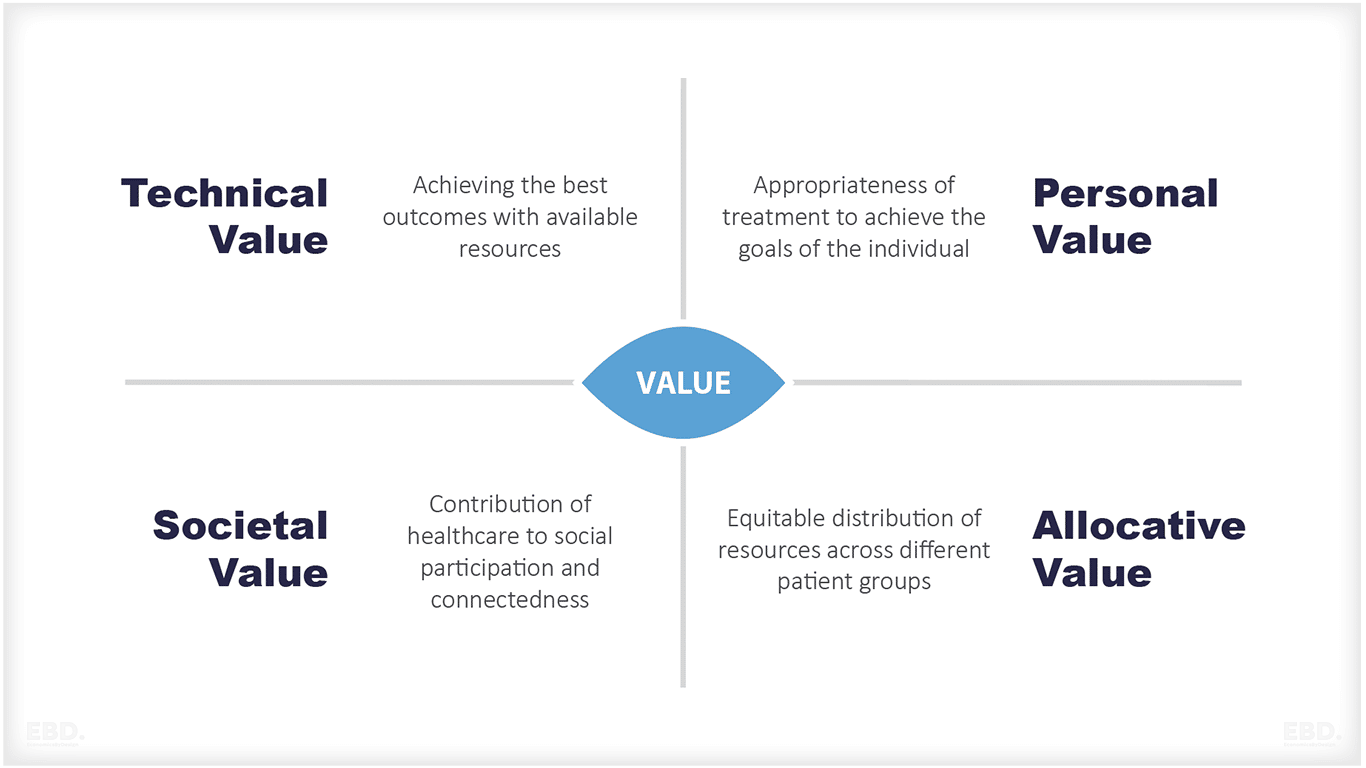
The European Commission Expert Panel takes this one step further and proposes four key value pillars:
- appropriate care to achieve patients’ personal goals (personal value),
- achievement of best possible outcomes with available resources (technical value),
- equitable resource distribution across all patient groups (allocative value) and
- contribution of healthcare to social participation and connectedness (societal value).
Strategic purchasing for UHC needs an effective purchasing system which considers all these elements and adopts a systems approach that accounts for the interconnectedness of different health services and the need for them to be integrated to be effective.
There are key principles that should guide strategic purchasing for UHC:
Alignment with national health priorities
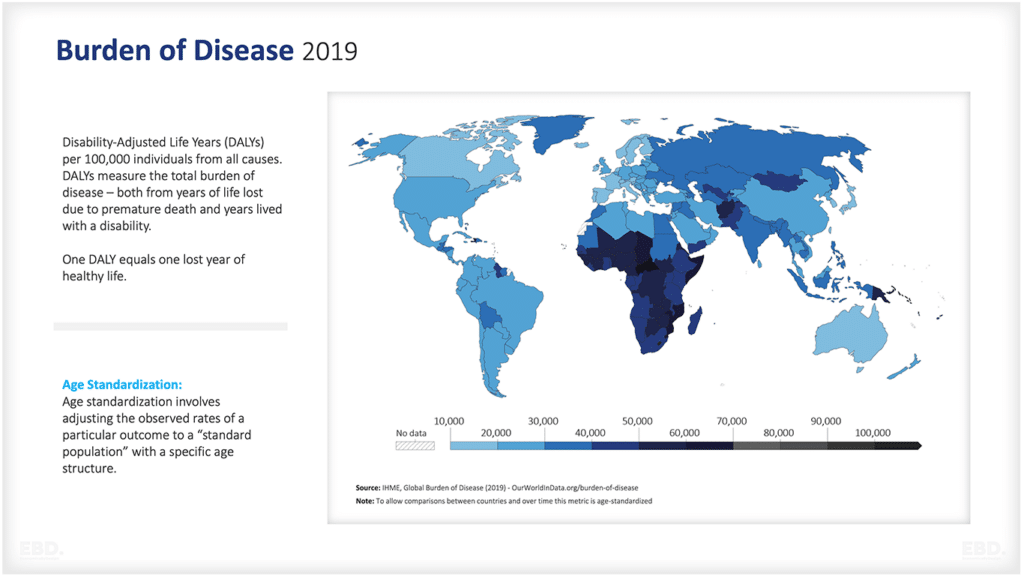
Purchasing decisions should be aligned with the overall health priorities of the country. This means considering factors such as disease burden, health workforce needs and equity considerations.
Long-term planning
Strategic purchasing requires long-term planning to ensure that the right mix of health services is procured to meet the needs of the population. This includes planning for future health needs and anticipated changes in disease patterns.
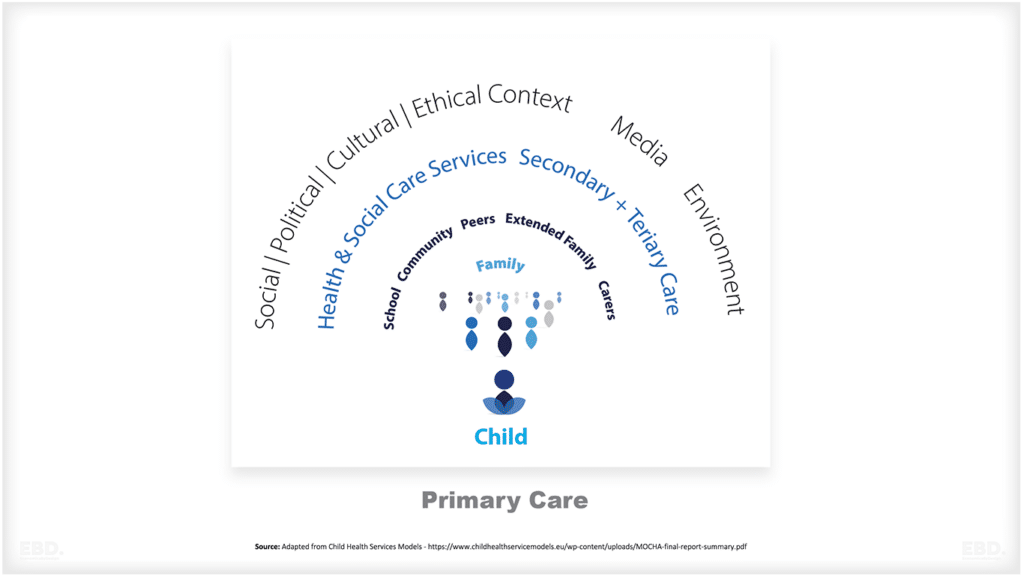
Purchasing decisions should also be based on an understanding of the drivers of health and disease in the population. This includes social determinants of health, such as education, housing and nutrition. Examples include investing in school health programs to improve child health or procuring community-based services to address social determinants of health.
Provider performance
Purchasing decisions should be based on an assessment of provider performance. This includes considering factors such as quality of care, cost-effectiveness and patient satisfaction.
Strategic purchasing often requires some form of provider accreditation or certification to ensure that standards are met. This should also include an independent inspection and monitoring of provider performance. Examples include accreditation of hospitals by the Joint Commission International (JCI) or HealthCERT in New Zealand.
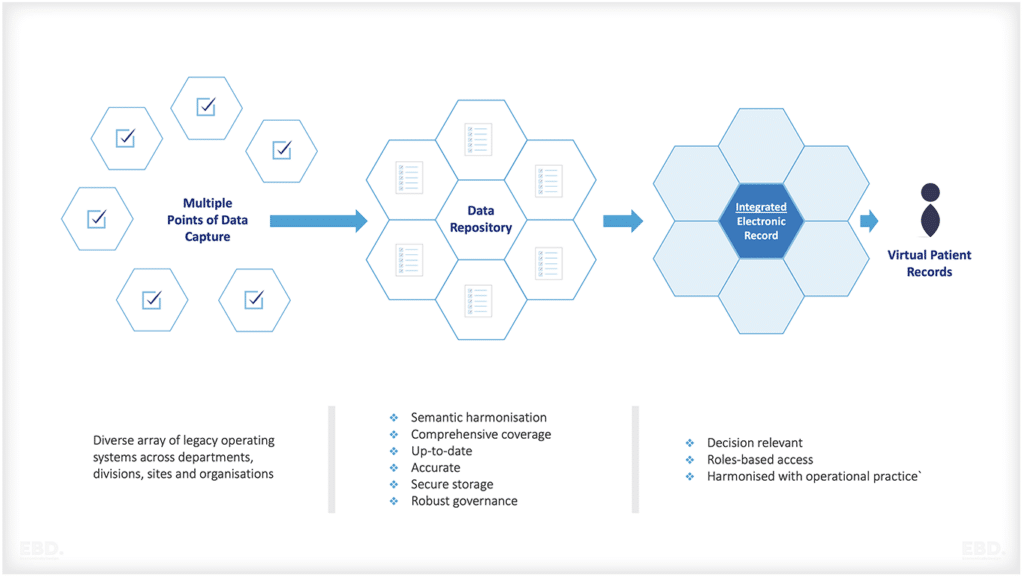
Use of data
Data should be used to inform purchasing decisions, with a focus on using real-time data to assess need and identify gaps in service provision. Data can also be used to monitor provider performance and assess the impact of purchasing decisions on health outcomes.
Examples, where data is used to inform purchasing decisions, include:
Payer claims data
This is data on the healthcare services that are provided to patients and paid for by insurers. It can be used to identify patterns of care, gaps in service provision and areas where quality improvement is needed.
Provider performance data
This is data on the quality of care provided by healthcare providers. It can be used to assess provider performance, identify areas for quality improvement and compare providers.
Patient satisfaction data
This is data on patients’ experiences of care. It can be used to assess patient satisfaction, identify areas for quality improvement and compare providers.
Health outcomes data
This is data on the health of populations. It can be used to assess the impact of purchasing decisions on health outcomes and to identify areas where improvements are needed.
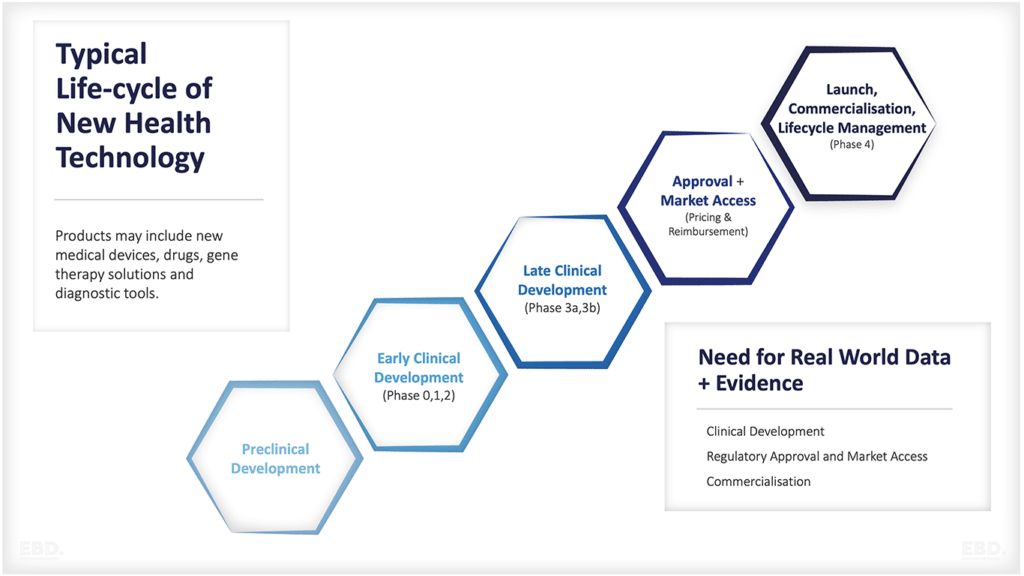
Use of evidence
Purchasing decisions should be based on the best available evidence. This includes both clinical and economic evidence. The use of clinical guidelines can help to ensure that purchasing decisions are based on the best available evidence.
Health Technology Appraisal (HTA) is another example of how evidence can be used in decision-making. In HTA, the clinical and economic evidence for health technology is appraised to inform purchasing decisions. A well-known example is the National Institute of Health and Care Excellence (NICE) in the UK which provides guidance on care pathways and the use of clinically effective health technologies.
Engagement of stakeholders
Strategic purchasing for UHC requires the engagement of all relevant stakeholders. This includes clinicians, managers, policy-makers and the general public. Engagement of all stakeholders is important to ensure that purchasing decisions are made in a transparent and accountable way. It is also important to ensure that all stakeholders have a clear understanding of the role of strategic purchasing in UHC.
Purchasing decisions should be based on the needs and preferences of patients and the general public. This can be done through the use of Patient and Public Involvement (PPI) techniques such as focus groups, patient surveys or citizen juries. PPI can help to ensure that purchasing decisions are made in a way that is responsive to the needs of the population.
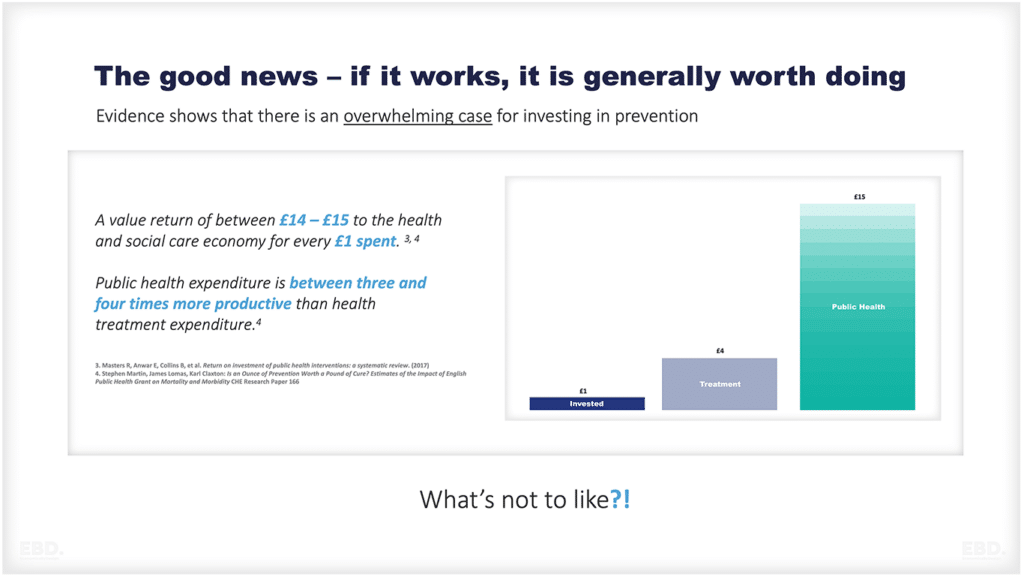
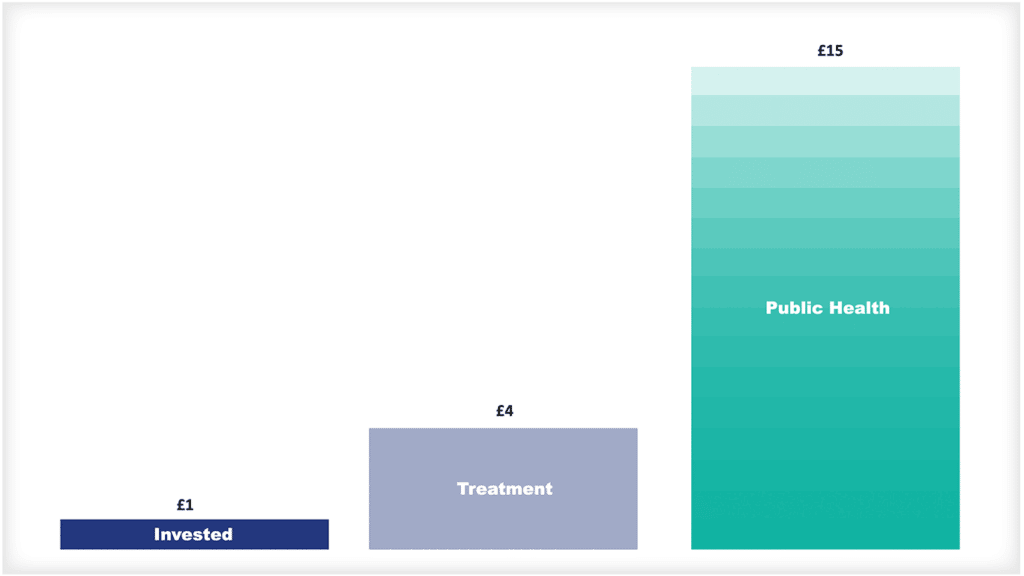
Value for money
Purchasing decisions should consider the cost-effectiveness of different health interventions. This means considering both the costs and health outcomes of different options. Cost-effectiveness analysis can help to inform purchasing decisions by providing a systematic way of comparing the costs and health outcomes of different options. Examples include the use of cost-effectiveness analysis to inform decision-making on the use of new drugs or health technologies as is done by NICE. Similar examples exist across Europe and increasingly globally.
Equity
Purchasing decisions should consider equity implications. This means taking into account how different interventions will impact different population groups. For example, some interventions may be more effective in reducing health inequalities if they are targeted at high-risk groups.
Incentivizing quality
Purchasing arrangements should incentivize quality, with a focus on rewarding providers for improving outcomes and providing high-quality care.
Foster competition
Where appropriate, competition among providers should be fostered to drive down costs and improve quality. This can be done through the use of tendering processes and other mechanisms.
Countries using strategic purchasing
In low-and middle-income countries (LMICs), the use of strategic purchasing to improve health outcomes is still in its early stages. Countries are beginning to explore how best to align purchasing decisions with national health priorities and move towards a more strategic approach. These include Ghana, Kenya, Rwanda, Tanzania and Uganda.
In upper-middle-income countries (UMICs), strategic purchasing is more established, with several countries having made significant progress in this area. These include Brazil, Mexico and Thailand.
In high-income countries (HICs), the use of strategic purchasing to improve health outcomes is well established. These include Australia, Canada, England, Scotland, Germany, the Netherlands Ireland, and the United States.
What are the governance challenges with strategic purchasing?
In many countries, there are many purchasing agencies engaged in the health system. These might be national or sub-national government agencies, social insurance organisations, private insurance companies, or donor agencies. Often these differ in terms of their goals and incentives and coordination across these multiple purchasers is almost impossible.
The WHO has set out nine governance requirements for strategic purchasing. These include:
1. Clear and consistent decision-making rules related to purchasing for the Ministry of Health, oversight body and purchaser
2. Public interest mandate and clear objectives to give the purchaser strategic direction and to act strategically
3. Sufficient autonomy and authority for the purchaser to act strategically to meet objectives, commensurate with the capacity
4. Effective oversight
5. Inclusive and meaningful stakeholder participation
6. Coherent multiple accountability lines supporting transparency
7. Firm and credible budget constraint
8. Selection of head of purchasing agency based on appropriate skills and performance incentives to guide operations
9. Compliance rules relating to the management and control of funds by the purchaser.
Where there are multiple actors involved there are also lots of risks largely resulting from diluted accountability.
The important relationship between the purchaser and the provider
Ultimately, the relationship between health purchasers and health providers is crucial in determining whether the system is effective in achieving improved health outcomes. The key issue here is one of aligning incentives so that providers are rewarded for delivering high-quality care, rather than simply providing more care.
Health Service Procurement
Government or insurance companies responsible for purchasing health services will need to identify and contract with health care providers. The process by which they engage with providers is known as procurement, and the agreements they reach are known as contracts.
The term procurement is sometimes used interchangeably with purchasing, but there is a difference between the two. Purchasing refers to the act of buying goods or services, while procurement refers to the process of acquiring goods or services.
Arrangements for procurement and contracting will vary depending on whether the purchaser is part of the public sector, using government or public funds, and whether the provider is an independent organisation.
In the public sector, procurement is usually governed by public contracting laws, such as the Federal Acquisition Regulation in the United States, or the European Union public procurement rules. These set out processes and regulations for contracting between agencies and vendors. Procurement laws exist to ensure that government agencies awarding contracts follow a fair and transparent process. The laws also aim to promote competition and protect the interests of taxpayers and mitigate the risks of corruption.
What are the different types of procurement?
There are many different types of procurement, but some common examples include:
Open Procurement
Also known as competitive bidding, open procurement is the most common type of procurement. In this process, vendors submit sealed bids to the contracting agency, and the agency awards the contract to the vendor with the lowest bid.
Limited Procurement
Limited procurement is used when there are only a few vendors who can provide the goods or services being procured. In this case, the contracting agency may choose to negotiate directly with the vendor rather than holding an open bidding process.
Direct Purchase
Direct purchase is used when the contracting agency needs to procure goods or services quickly and there is only one vendor who can provide them. In this case, the contracting agency may choose to bypass the bidding process and purchase the goods or services directly from the vendor.
Many different factors must be considered in any procurement, such as cost, quality, delivery time, and so on. The type of procurement that is used will often depend on these factors.
What are procurement thresholds?
Procurement thresholds are the monetary limits set by governments or other organizations for the value of goods, services, or works that can be procured without a formal tendering process. For example, in the European Union, the procurement threshold for goods and services is €140,000, while the threshold for public works contracts is €5,382,000.
Procurement thresholds vary from country to country and organization to organization. They are usually set based on the value of the contract, but may also be based on the type of goods or services being procured.
What is the health system supply chain?
The supply chain covers the network of organizations and activities involved in the procurement, distribution, and use of goods and services needed to deliver health care. The supply chain begins with the manufacturers of goods and services and ends with the patients who receive them.
In between are a variety of suppliers, distributors, wholesalers, retailers, and other organizations. It is a global network of organizations and activities. It is subject to a variety of risks, such as delays in delivery, shortages of supplies, and price fluctuations. Often health service providers along the supply chain need to be accredited to provide health services and are subject to regulation and inspection.
In this context, service providers also procure. Health care service providers can use their own “buying power” to get the best value from supplies and critical infrastructure. They will often have their own procurement departments and, if accountable to the public sector, will often have to abide by the same procurement rules and thresholds.
In some countries, such as the UK, where the majority of providers are publicly owned, a selection of commonly used medical supplies procured by health service providers, will be governed by national prices negotiated by the purchaser. This often applies to pharmaceutical products and medical devices.
One of the main challenges in low to middle-income countries is that procurement systems are often not well developed. This can lead to corruption and inefficiency. In addition, there may be a lack of capacity within the Procurement function, which can further contribute to these problems. As a result, it is often difficult for purchasers in these countries to get the best value for money when procuring goods and services.
What are the Economic Impacts of an Effective Procurement System?
There are several economic impacts of an effective procurement system. One impact is that it can help to ensure that goods and services are procured efficiently. This can save significant amounts of money for purchasers, as well as for patients and taxpayers.
Another impact is that it can help to ensure that goods and services are procured ethically and sustainably. This can create jobs and business opportunities, as well as help to protect the environment.