Introduction to Health System Goals
Health system goals are the objectives that a healthcare system sets to improve the population health and the performance of the health system. These goals can be set at different levels, from global to national to local.
Global health outcome targets, set by the United Nations, include, for example:
- reducing maternal mortality
- reducing preventable deaths for children under the age of 5
- reducing the risk of communicable disease
- reduce deaths and injuries from road traffic accidents
However, there is no international consensus on how best to measure health system performance.
Country context matters and the current state of population health and health system maturity has a huge impact on what goals can be set and what might feasibly be achieved.
At the national level, healthcare system goals will vary depending on the specific needs of a country. However, some common goals that might be set at this level include improving access to healthcare, increasing the quality of care, and reducing healthcare costs.
Local health system goals will also vary depending on the needs of a specific community or population. However, some common goals that might be set at this level include increasing the number of people who receive preventive care, reducing health disparities, and improving the coordination of care.
This article explores the different types of goals of health systems and how they are measured.
What are the 13 Global Health Targets
In 2015, the United Nations set 17 goals for Sustainable Development by 2030 many of which impact health and well-being.
Sustainable Development Goal 3 (SDG 3) is to
“ensure healthy lives and promote well-being for all at all ages”.
There are 13 targets:
- By 2030, reduce the global maternal mortality ratio to less than 70 per 100,000 live births
2.By 2030, end preventable deaths of newborns and children under 5 years of age, with all countries aiming to reduce neonatal mortality to at least as low as 12 per 1,000 live births and under-5 mortality to at least as low as 25 per 1,000 live births
- By 2030, end the epidemics of AIDS, tuberculosis, malaria and neglected tropical diseases and combat hepatitis, water-borne diseases and other communicable diseases
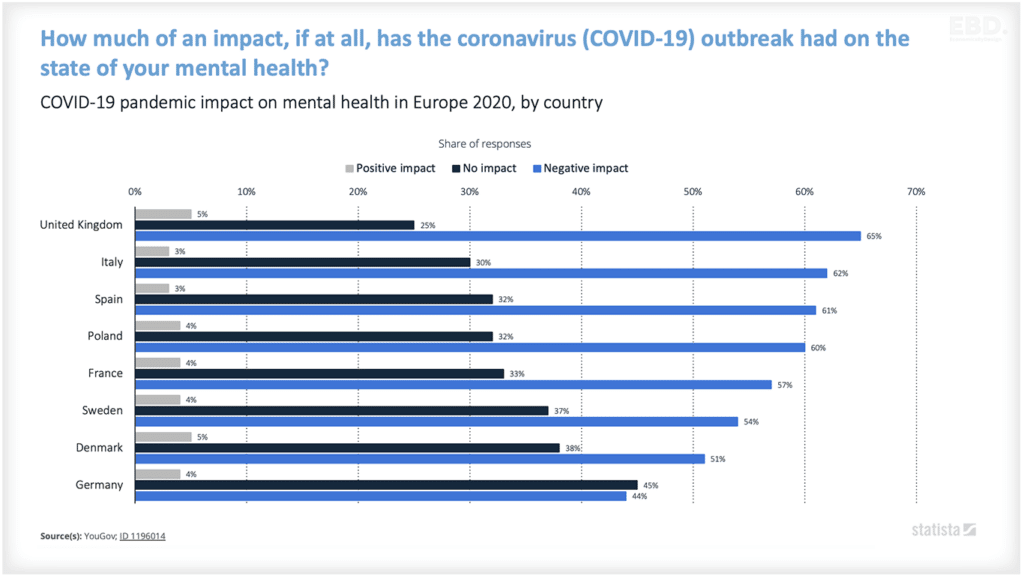
- By 2030, reduce by one third premature mortalities from non-communicable diseases through prevention and treatment and promote mental health and well-being
- By 2030, strengthen the prevention and treatment of substance abuse, including narcotic drug abuse and harmful use of alcohol.
- By 2030, halve the number of global deaths and injuries from road traffic accidents
- By 2030, ensure universal access to sexual and reproductive health-care services, including for family planning, information and education, and the integration of reproductive health into national strategies and programmes.
- Achieve universal health coverage, including financial risk protection, access to quality essential health-care services and access to safe, effective, quality and affordable essential medicines and vaccines for all.
- By 2030, substantially reduce the number of deaths and illnesses from hazardous chemicals and air, water and soil pollution and contamination.
- By 2030, substantially reduce the number of deaths and illnesses from hazardous chemicals and air, water and soil pollution and contamination
- Strengthen the implementation of the World Health Organization Framework Convention on Tobacco Control in all countries as appropriate
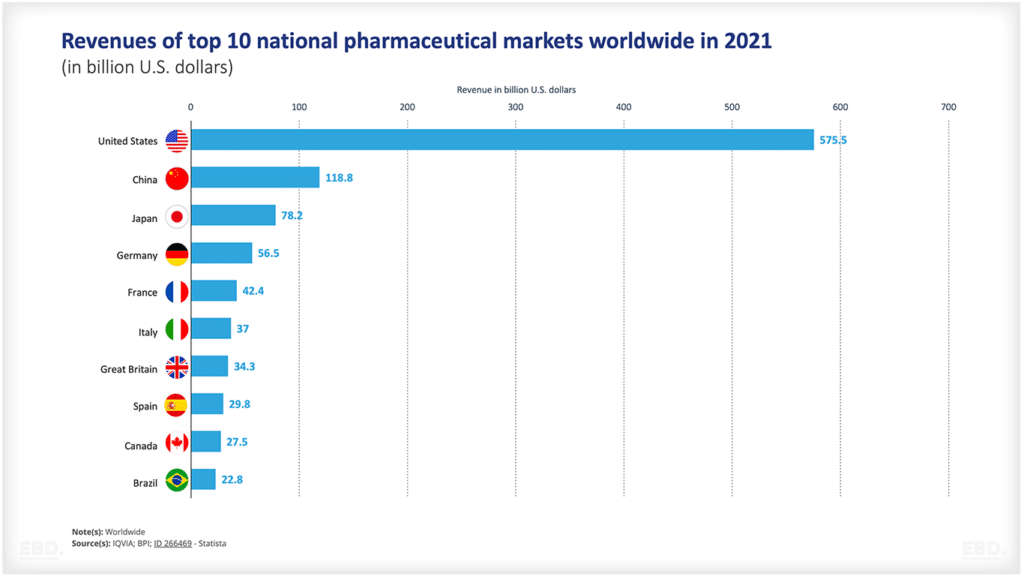
- Support the research and development of vaccines and medicines for the communicable and non-communicable diseases that primarily affect developing countries, provide access to affordable essential medicines and vaccines, in accordance with the Doha Declaration on the TRIPS Agreement and Public Health, which affirms the right of developing countries to use to the full the provisions in the Agreement on Trade-Related Aspects of Intellectual Property Rights regarding flexibilities to protect public health, and, in particular, provide access to medicines for all.
- Strengthen the capacity of all countries, in particular developing countries, for early warning, risk reduction and management of national and global health risks.
There are many more health-related targets in the Sustainable Development Goals such as improving diet and food security, access to education, access to safe water etc.
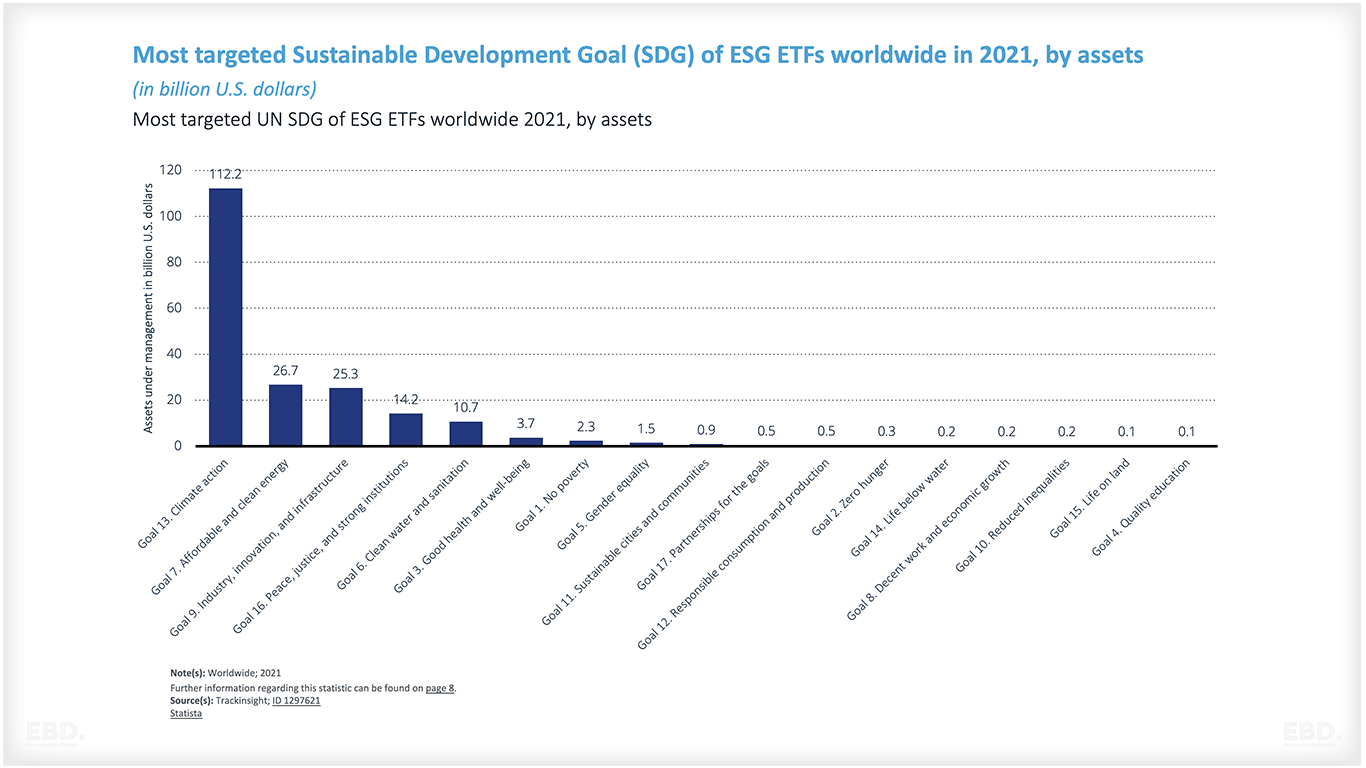
SDG 3 is ranked 6th out of the 17 SDGs in terms of investment in Environmental Social and Governance Exchange Trading Funds (ETF) in 2021 globally.
The Global Action Plan for Healthy Lives and Well-being for All (SGD3 GAP) involves 13 global partners and agencies and was established to support governments to achieve health-related Sustainable Development Goals.
What Are Some Common National Health System Goals?
There are a variety of different types of goals that health systems may set at different levels. Some examples of healthcare system goals include:
- Improving access to healthcare: This might involve increasing the number of primary care providers in a community or ensuring that all residents have health insurance.
- Improving the quality of care: This might involve increasing patient safety or ensuring that all patients receive evidence-based care.
- Reducing healthcare costs: This might involve reducing unnecessary testing and procedures or improving the efficiency of the healthcare system.
- Reducing health disparities: This might involve increasing the number of minority residents who receive preventive care or providing culturally competent care to all patients.
- Improving the coordination of care: This might involve increasing the number of patients who see a primary care provider on a regular basis or ensuring that all patients have a medical home.
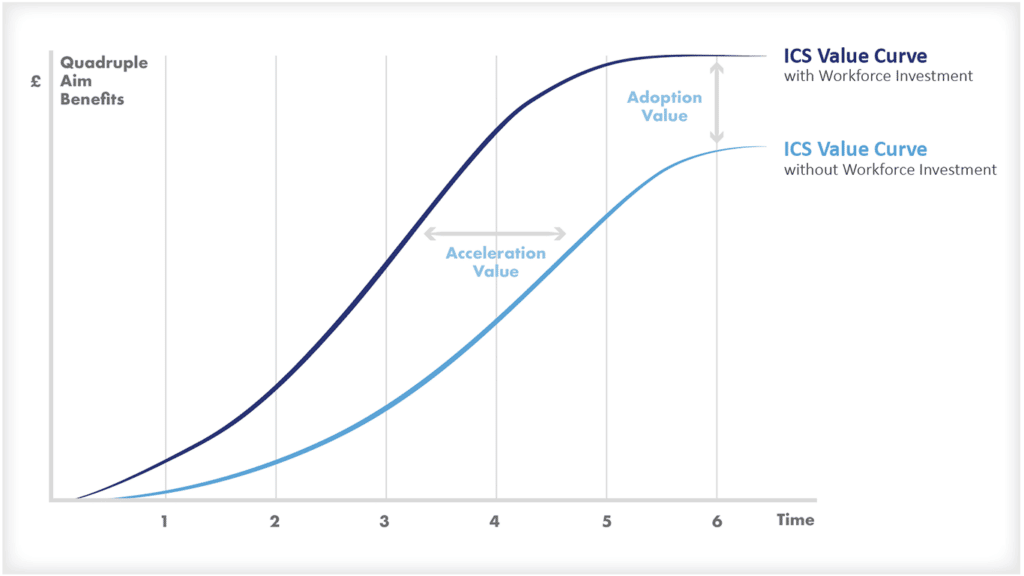
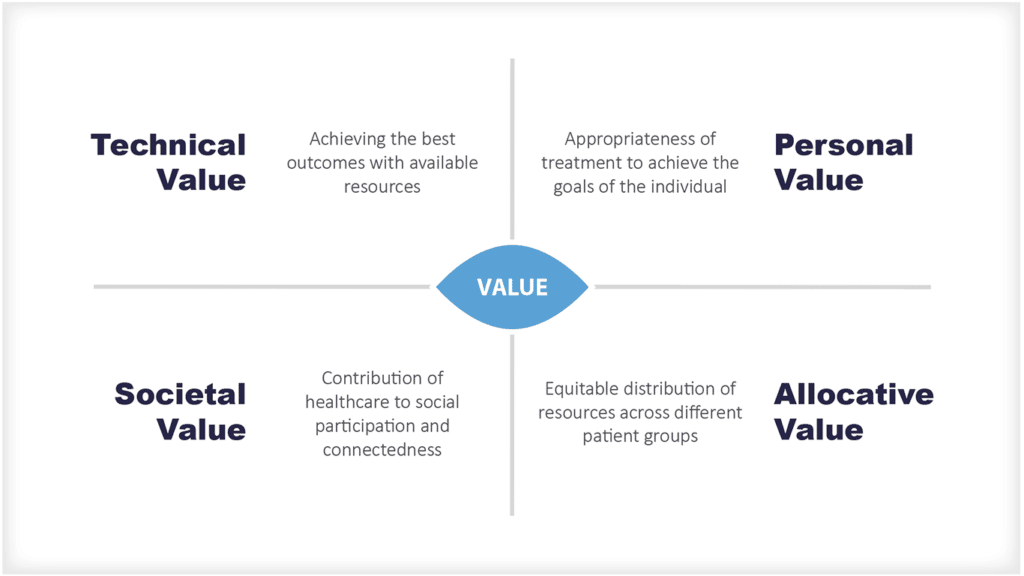
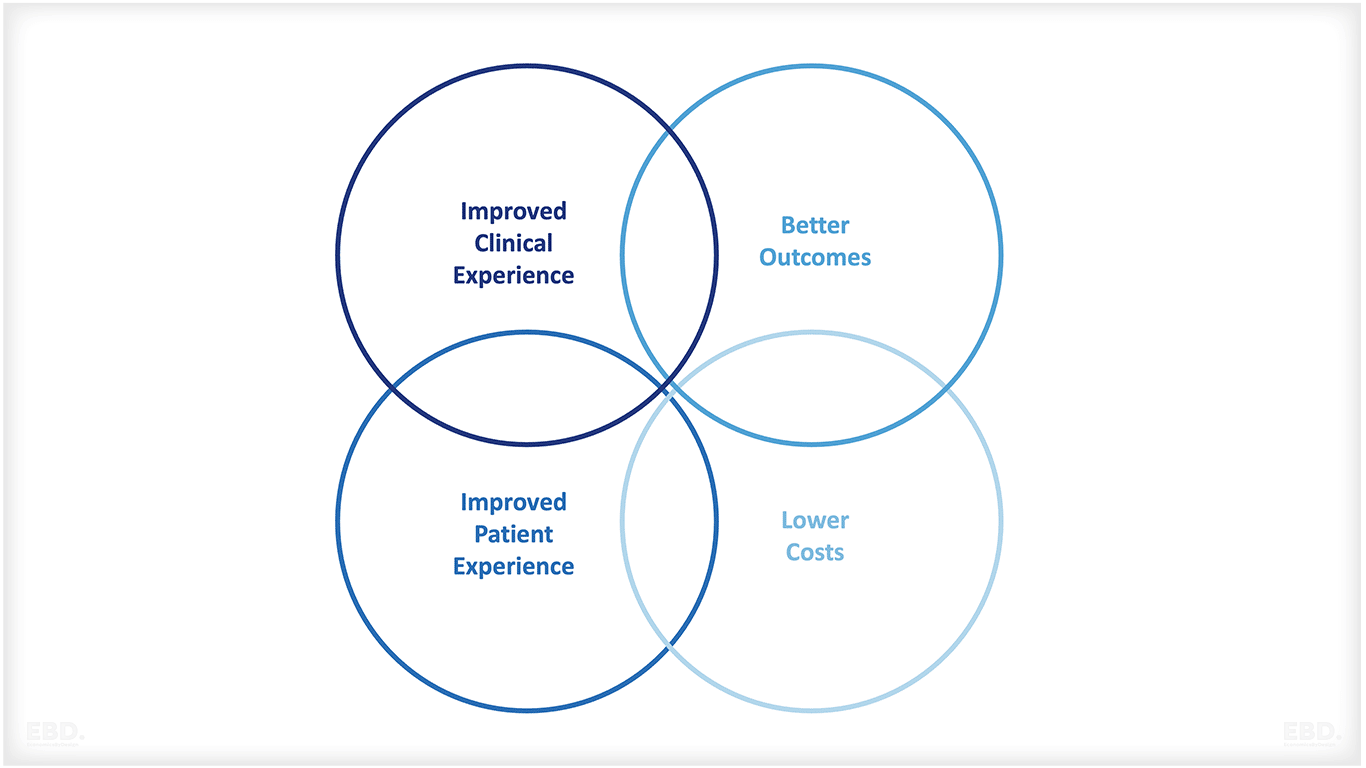
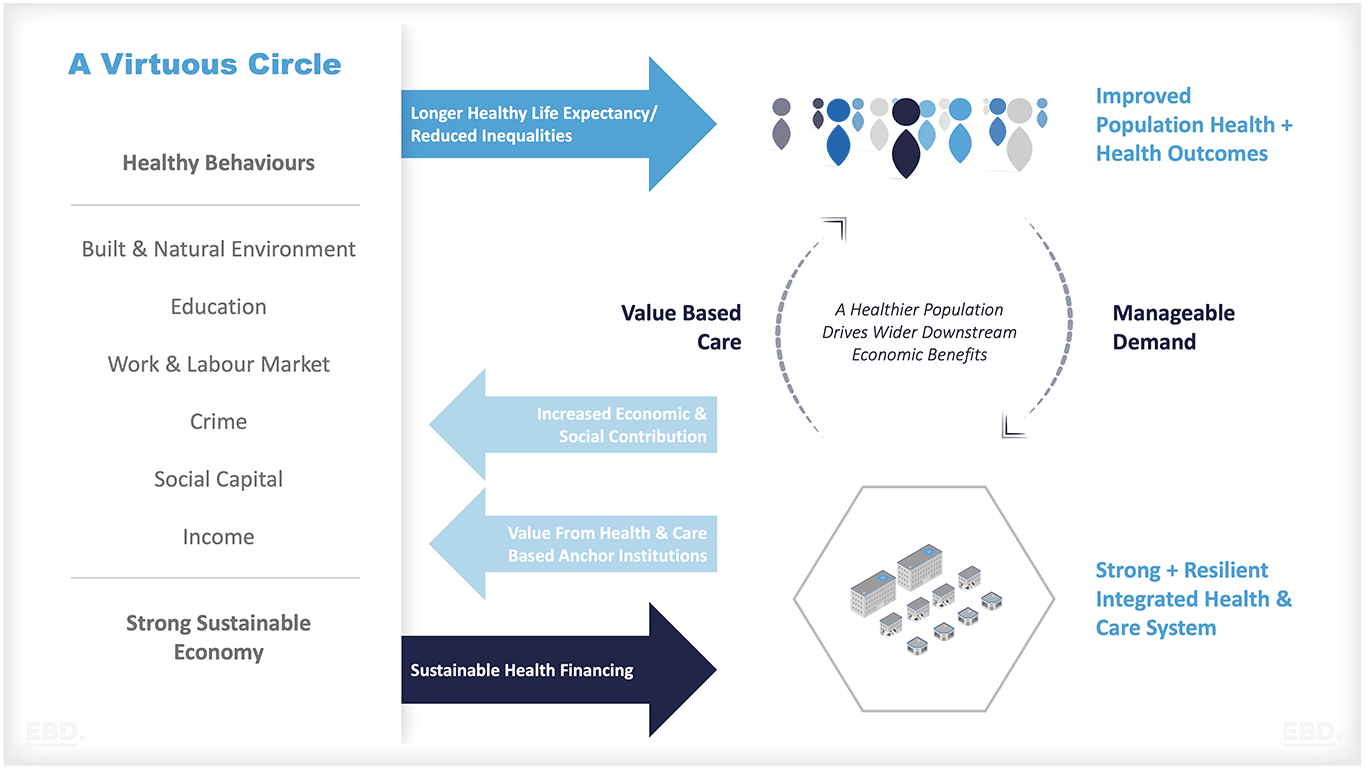
Health systems are increasingly using value-based healthcare frameworks such as the triple aim or the quadruple aim to frame national health system goals.
Health outcomes
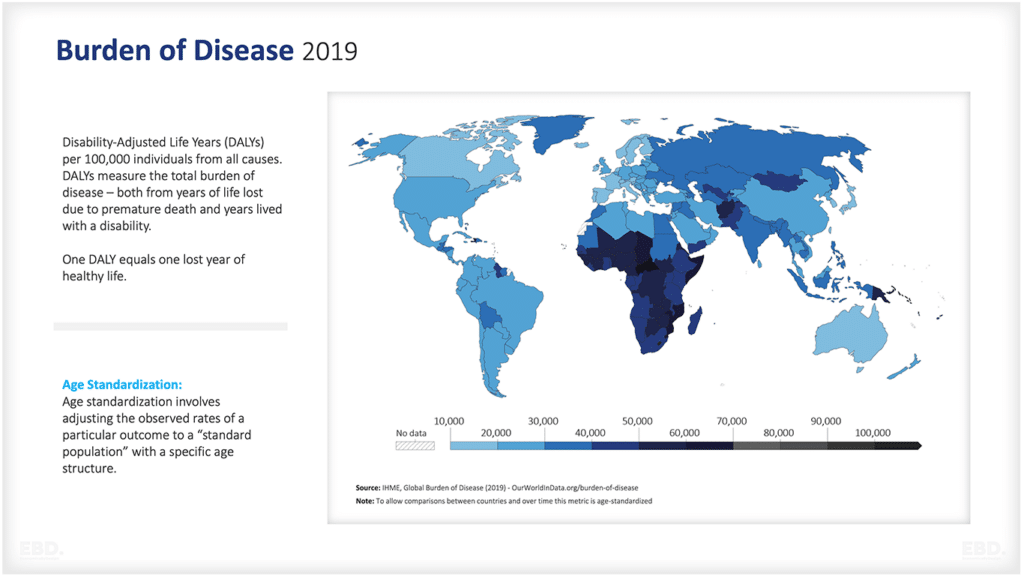
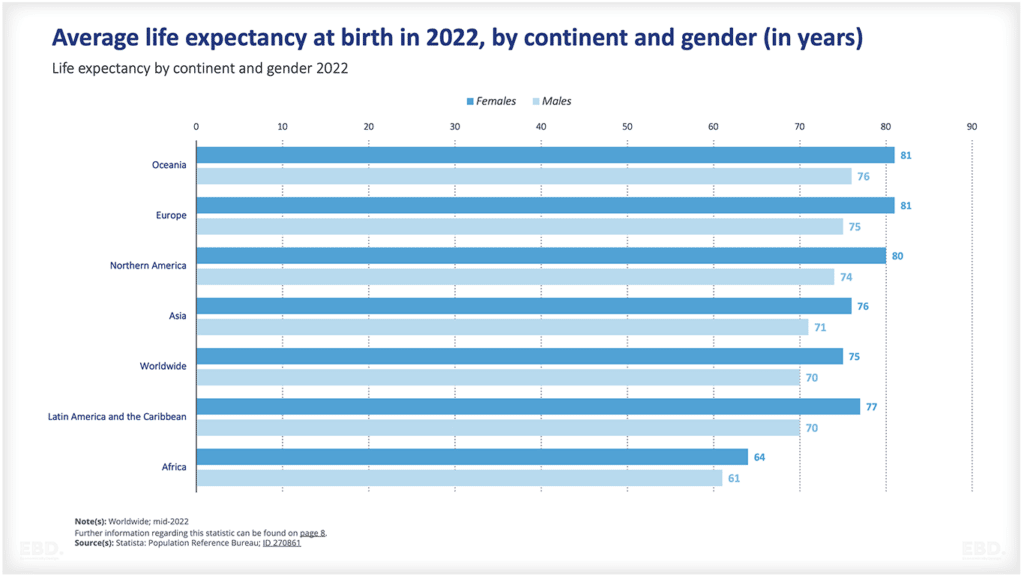
The World Health Organization (WHO) defines health outcomes as “the health status of a person or population at a specific point in time, or over a period of time, which can be measured using various indicators.” In other words, health outcomes are the end result of a person’s or population’s health status.
There are many different types of health outcomes, but they can be broadly classified into two main categories: mortality outcomes and morbidity outcomes.
Mortality outcomes
These refer to the number of deaths that occur within a population over a specific period. These outcomes can be further sub-categorized into all-cause mortality (the total number of deaths from all causes) and cause-specific mortality (the number of deaths from a specific cause).
Morbidity outcomes
These refer to the number of people within a population who experience a particular health condition or disease over a specific period. Morbidity can be measured in terms of prevalence (the number of people with a condition at a given point in time) or incidence (the number of new cases of a condition over a given period of time).
Health outcomes are important because they provide a measure of whether or not the health of a population is improving, worsening, or remaining stable over time. They also allow comparisons to be made between different populations (for example, between different countries or regions) and can help to identify areas where intervention is needed in order to improve the health of a population.
Many different factors can impact health outcomes. These include but are not limited to:
- The quality of healthcare: This includes factors such as the availability of preventive care and treatment, the effectiveness of care, and patient safety.
- Socioeconomic status: This refers to factors such as income, education, and employment. It is well-established that people with lower socioeconomic status are more likely to experience poorer health outcomes.
- The social determinants of health: These are the conditions in which people live, work, and play. They include factors such as housing, transportation, and access to healthy food. The social determinants of health have a significant impact on health outcomes.
- Health risk factors: These are the behaviours and conditions that increase the likelihood of developing a disease or experiencing an adverse health event. Common examples of health risk factors include smoking, obesity, and high blood pressure.
The above list is by no means exhaustive but provides a general overview of some of the main factors that can influence health outcomes.
What Are Some Challenges Associated With Setting Healthcare System Goals?
There are many challenges associated with setting healthcare system goals. These challenges include but are not limited to:
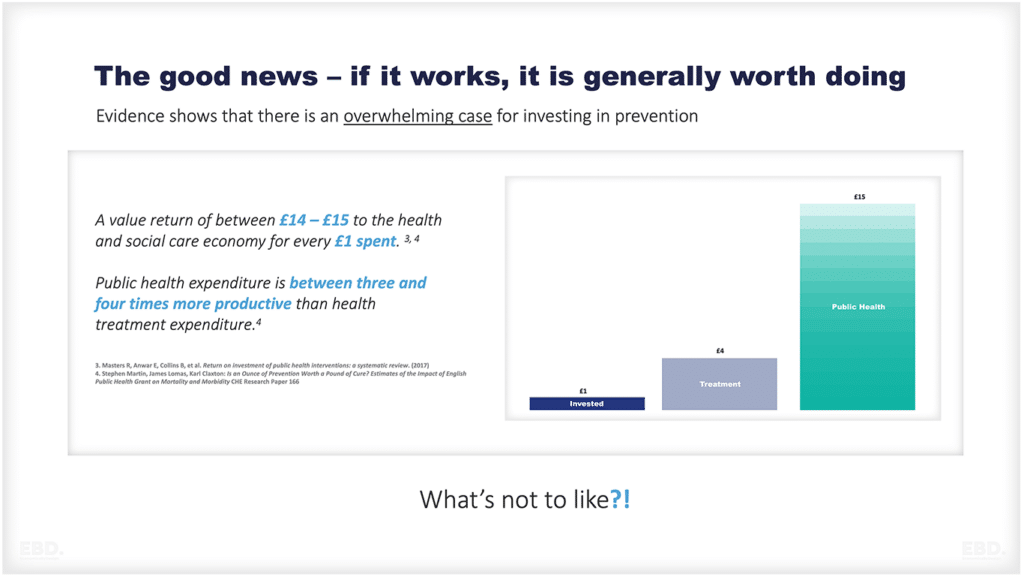
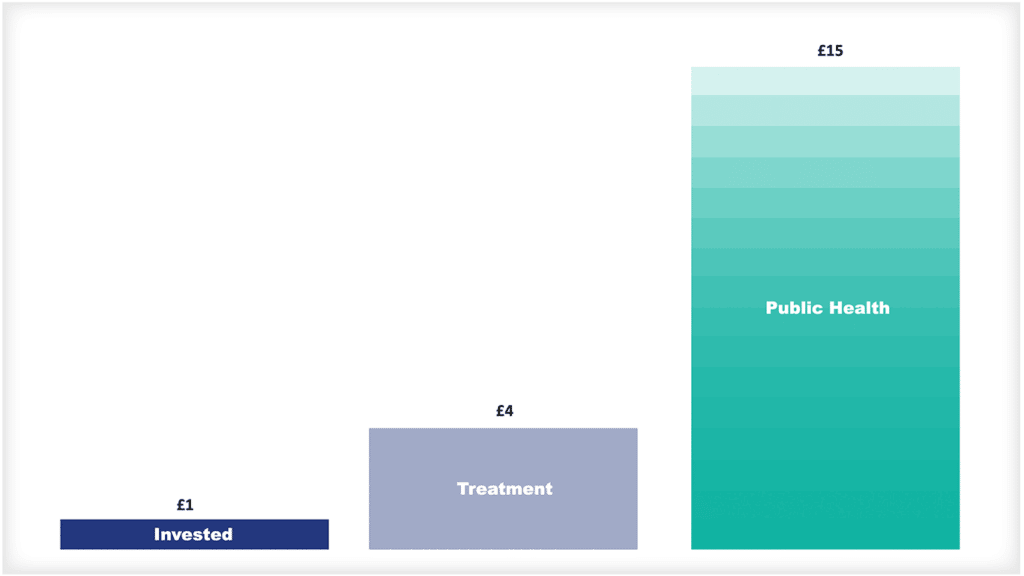
Cost
Many healthcare interventions can be costly, and it can be difficult to find the resources to implement them on a wide scale.
Feasibility
Some healthcare interventions might not be feasible to implement in a given setting. For example, an intervention that requires a high level of resources might not be feasible to implement in a resource-poor setting.
Sustainability
It can be difficult to sustain healthcare interventions over the long term. This is often due to factors such as changes in funding or staffing levels.
Evaluation
It can be difficult to evaluate the impact of healthcare interventions, particularly when multiple factors can influence health outcomes.
Political will
There needs to be sufficient levels of political will to implement healthcare interventions on a wide scale. This can be difficult to achieve, particularly in the face of competing priorities.
Despite these challenges, it is important to set healthcare system goals in order to improve the health of a population. Goal-setting can help to focus attention and resources on priority health issues, and it can provide a framework for evaluating the impact of healthcare interventions.
What Are Some Tips For Setting Healthcare System Goals?
There are a number of things to consider when setting healthcare system goals. These tips can help to ensure that goals are realistic and achievable:
Consult with stakeholders
It is important to consult with key stakeholders when setting healthcare system goals. This will help to ensure that goals are aligned with the needs of the population.
Set Realistic Goals
It is important to set realistic goals that can be achieved within a reasonable timeframe. Setting unrealistic goals can lead to frustration and disillusionment.
Be Specific
Goals should be specific in order to be measurable. For example, rather than setting a goal of “improving access to healthcare,” a more specific goal might be “increasing the number of primary care providers in a community.”
Make Use of Existing Data
When setting healthcare system goals, make use of existing data sources such as national health surveys. This will help to ensure that goals are evidence-based.
Seek Input From Experts
When setting healthcare system goals, seek input from experts in the field. This will help to ensure that goals are achievable and realistic.
What Are Some Examples of Healthcare System Goals?
There are a number of possible healthcare system goals that could be set. These goals might focus on improving the quality of care, reducing healthcare costs, or reducing health disparities. Some examples of healthcare system goals include:
- Increasing the number of primary care providers in a community.
- Ensuring that all patients receive evidence-based care.
- Reducing unnecessary testing and procedures.
- Improving the efficiency of the healthcare system.
- Increasing the percentage of patients who receive preventive care.
- Reducing health disparities among different population groups.
- Improving the quality of care for chronic conditions.
- Reducing the rate of hospital readmissions.
- Increasing patient satisfaction with the healthcare system.
- Improving population health outcomes.
It is important to set healthcare system goals that are evidence-based and achievable. However, it is also important to be aware of the challenges that can be associated with goal-setting. These challenges include feasibility, cost-effectiveness, and equity.
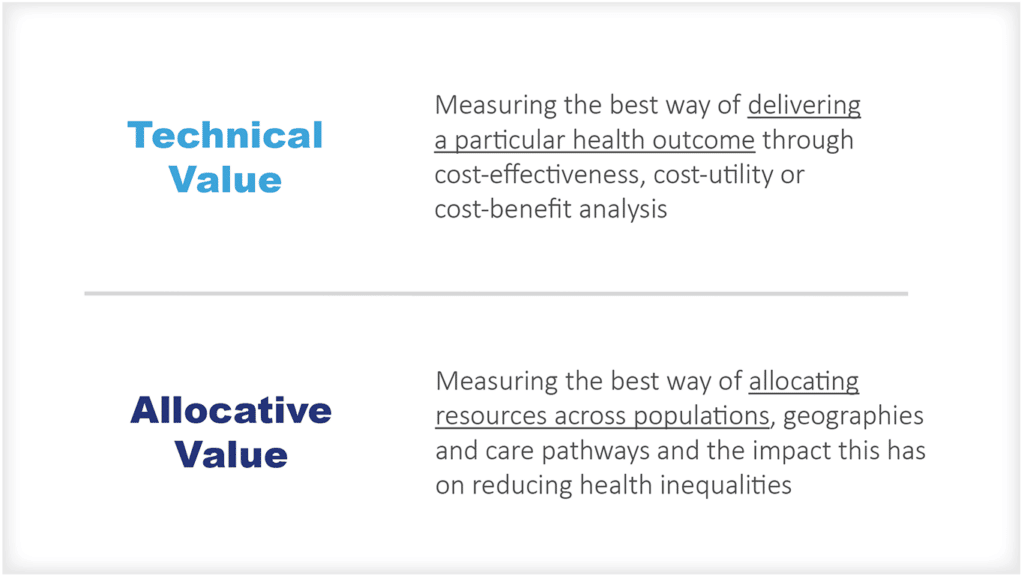
Value-based Healthcare and Health Outcomes
Value-based healthcare is an approach to healthcare that focuses on improving patient outcomes. This means that rather than simply focusing on the provision of care, value-based healthcare also takes into account the health outcomes of patients.
One example of a value-based healthcare goal might be to reduce the number of hospital readmissions. This goal would focus on improving patient outcomes by ensuring that patients are not discharged too early and then requiring readmission.
Another example might be to improve population health outcomes at the citizen level. This could involve setting goals such as reducing smoking rates or increasing vaccination rates.
Achieving these kinds of goals can require a multi-sectoral approach, as well as a focus on health promotion and disease prevention. It is important to remember that these kinds of goals require a long-term commitment and cannot be achieved overnight.
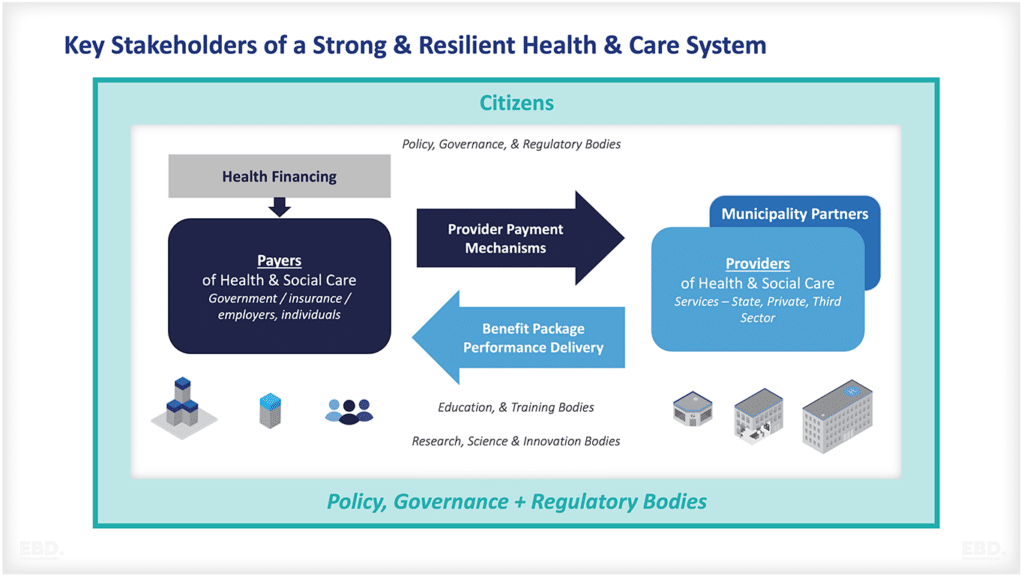
When setting healthcare system goals, it is important to consider the needs of all stakeholders. This includes patients, providers, payers, and the community. Goals should be achievable and realistic, and they should be based on evidence.
Patient centred care
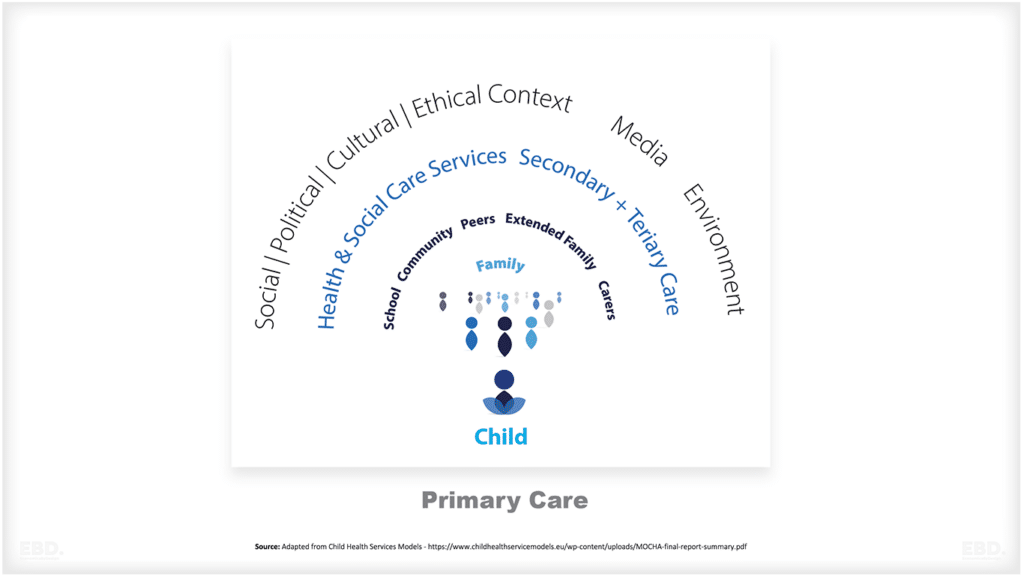
Patient-centered care is an approach to healthcare that focuses on meeting the needs of the patient. This means that rather than simply providing care, patient-centered care also takes into account the preferences and values of patients.
One example of a patient-centered goal might be to ensure that all patients have access to their medical records. This would allow patients to be more involved in their own healthcare and make informed decisions about their treatment.
Another example might be to improve communication between patients and providers. This could involve setting goals such as increasing the number of provider-patient visits that are conducted face-to-face, or ensuring that all phone calls and emails are returned within 24 hours.
Achieving these kinds of goals can require a change in the way that healthcare is delivered. It is important to remember that these kinds of goals require a long-term commitment and cannot be achieved overnight.
When setting healthcare system goals, it is important to consider the needs of all stakeholders. This includes patients, providers, payers, and the community. Goals should be achievable and realistic, and they should be based on evidence.
What are Patient Reported Outcome Metrics?
Patient Reported Outcome Metrics (PROMs) are a type of patient-centered metric that focus on the outcomes that are important to patients. This means that rather than simply measuring the provision of care, PROMs also take into account the health outcomes of patients.
An example might be to measure the number of patients who experience a health complication after discharge from the hospital. This could help to identify potential problems with the care that patients are receiving and make sure that they are getting the best possible care.
What are Patient Reported Experience Metrics?
Patient Reported Experience Metrics (PREMs) are a type of patient-centered metric that focus on the experiences of patients. This means that rather than simply measuring the provision of care, PREMs also take into account the way that patients feel about their care.
An example might be to measure the number of patients who are satisfied with the care that they received. This could help to identify areas where patients are not happy with their care and make sure that they are getting the best possible care.
What is the difference between a goal and a key performance indicator?
A goal is a desired outcome that healthcare organizations hope to achieve. Key performance indicators (KPIs) are a type of metric that is used to measure progress towards a goal. This means that KPIs can be used to track whether or not a healthcare organization is making progress towards its goals.
Health System Goals in England: A Case Study
The Department for Health and Social Care (DHSC) is responsible for setting policy for the health system in England. Its current priorities are to:
- protect the public’s health through the health and social care system’s response to COVID-19
- improve healthcare outcomes by providing high-quality and sustainable care at the right time in the right place and by improving infrastructure and transforming technology
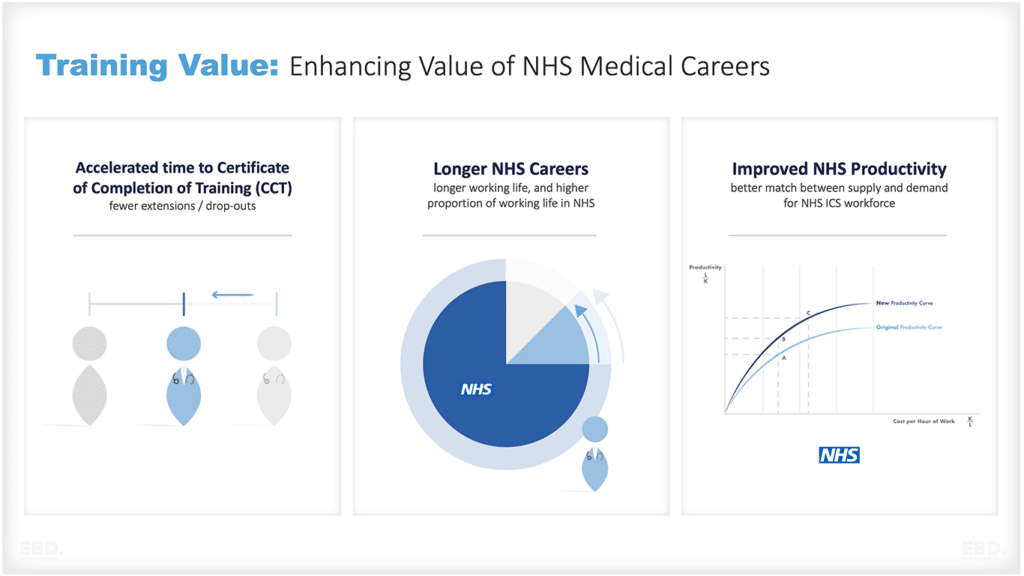
- improve healthcare outcomes through a well-supported workforce
- improve, protect and level up the nation’s health, including through reducing health disparities
- improve social care outcomes through an affordable, high quality and sustainable adult social care system
The latest plan published in September 2022, included goals to:
- ensure access to primary care – with appointment waiting times set at or below 2 weeks
- help individuals move from hospital to social care when they need it
- support clinicians to extend their careers and enhance the use of volunteers to support health services
NHS England is an executive non-departmental public body responsible for the NHS in England. It reports to the DHSC. The DHSC provides a mandate for NHS England to Deliver against national priorities.
For 2022-23, the 5 objectives set by the DHSC for NHS England were for it to:
- continue to lead the NHS in managing the impact of COVID-19 on health and care
- recover and maintain delivery of wider NHS services and functions
- renew focus on delivering against the NHS long-term plan and broader commitments for the NHS
- embed a population health management approach with local systems, stepping up action to prevent ill health and tackle health inequalities
- ensure effective NHS leadership, culture and use of organisational resource to realise the benefits from future structural changes within health and care
NHS England then sets goals and targets for the NHS in England. These are set out as operational planning guidance. For 2022-23, these were focused on:
- investment in the workforce
- even further improvements to the response to Covid-19, including vaccination and focusing on COVID-19 syndrome (long-covid)
- increase the delivery of elective or planned care to 110% of pre-pandemic levels so as to address the backlog and reduce long waiting times and to address particular challenges in relation to cancer, diagnostics and maternity care
- improve the responsiveness of urgent and emergency care including improving services in the community to enable more care to be delivered at home
- improve access to primary care
- improve mental health services and for people with a learning disability
- continuing to develop population health management approaches for improving health and reducing health inequalities
- achieve a core level of digitisation in every service
- revert to pre-pandemic levels of productivity
- the establishment of the 42 integrated care systems from July 2022.
Integrated Care Systems have been given 4 overall aims:
- Improve outcomes in population health and healthcare
- Tackle inequalities in outcomes, experience and access
- Enhance productivity and value for money
- Help the NHS support broader social and economic development
Each Integrated Care System will collaborate on setting local goals and targets for the geographies and organisations within the scope of their governance. This will include shared goals and targets for “place” and within these “neighbourhoods”. It will include goals for public health, health service delivery and social care.
In North West London for example, high level objectives have been set to:
- identify and address inequalities in access, experience and outcomes
- put in place the building blocks of a population health approach
- improve health and prevent illness as identified in Core20PLUS5
- improve social environmental and healthy living factors that adversely affect health and well-being
These goals will then cascade to the respective accountable organisation (the Local Authority and the Integrated Care Board) and through to providers through strategic purchasing and contracting.
NHS England has set 8 objectives for integrated care systems For winter 2022:
- Prepare for variants of COVID-19 and respiratory challenges, including an integrated COVID-19 and flu vaccination programme.
- Increase capacity outside acute trusts, including the scaling up of additional roles in primary care and releasing annual funding to support mental health through the winter.
- Increase resilience in NHS 111 and 999 services, through increasing the number of call handlers to 4.8k in 111 and 2.5k in 999.
- Target Category 2 response times and ambulance handover delays, including improved utilisation of urgent community response and rapid response services, the new digital intelligent routing platform, and direct support to the most challenged trusts.
- Reduce crowding in A&E departments and target the longest waits in ED, through improving use of the NHS directory of services, and increasing provision of same day emergency care and acute frailty services.
- Reduce hospital occupancy, through increasing capacity by the equivalent of at least 7,000 general and acute beds, through a mix of new physical beds, virtual wards, and improvements elsewhere in the pathway.
- Ensure timely discharge, across acute, mental health, and community settings, by working with social care partners and implementing the 10 best practice interventions through the ‘100 day challenge’.
- Provide better support for people at home, including the scaling up of virtual wards and additional support for High Intensity Users with complex needs.
These will be monitored using 6 metrics:
- 111 call abandonment. (111 is a telephone triage system for urgent care)
- Mean 999 call answering times. (999 is a telephone triage system for emergency services including ambulance services)
- Category 2 ambulance response times. (category 2 is an emergency or serious condition which may require rapid assessment, on-scene intervention, or urgent transport to the hospital)
- Average hours lost to ambulance handover delays per day.
- Adult general and acute type 1 bed occupancy (adjusted for void beds). (acute trusts with major emergency departments)
- Percentage of beds occupied by patients who no longer meet the criteria to reside.