What is a Health Economist?
A health economist is someone who is an expert in applying the principles of economics to healthcare. They use their skills to understand and analyze the complexities of the healthcare system, and to make recommendations on how to improve or invest in it.
They may work in a variety of settings, such as government agencies, think tanks, or private companies. In each case, their goal is to find ways to make the healthcare system more efficient and effective.
To understand why we have specialists in health economics, it is important to first understand some key principles of economics.
- Economic Value
- Scarcity
- Opportunity Cost
- Rationality
- Incentives
- Markets
- Market Failure
- Government
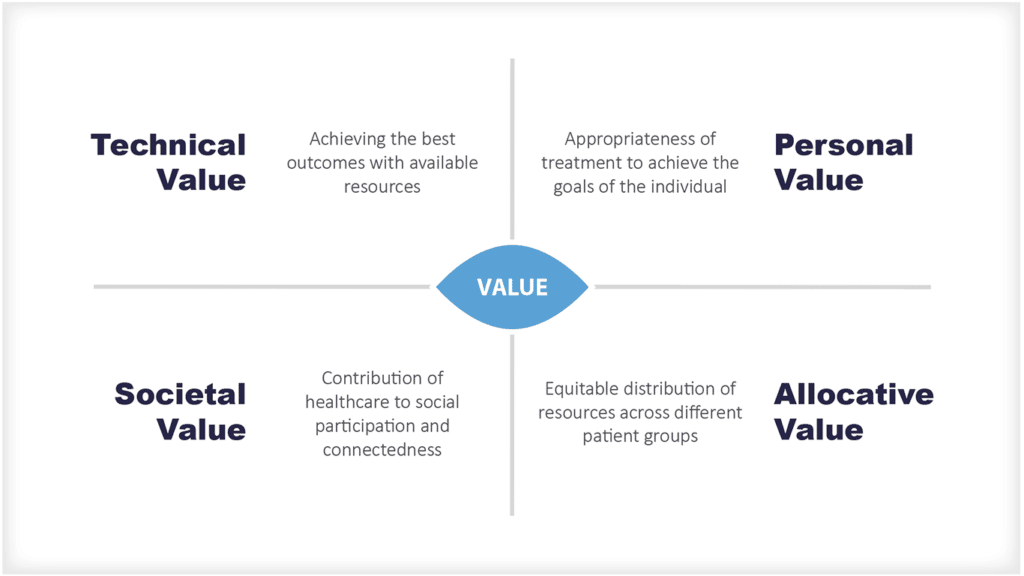
Economic Value
From a health economist’s perspective, everything we do has economic value. This may seem like a given, but it’s an important concept. Everything we do has an opportunity cost – meaning, there is always something else we could be doing with our time, money, and resources.
For example, if you choose to go to the cinema instead of going out to dinner, you are giving up the chance to have a nice meal. The cost of your cinema ticket is the opportunity cost of not going out to dinner
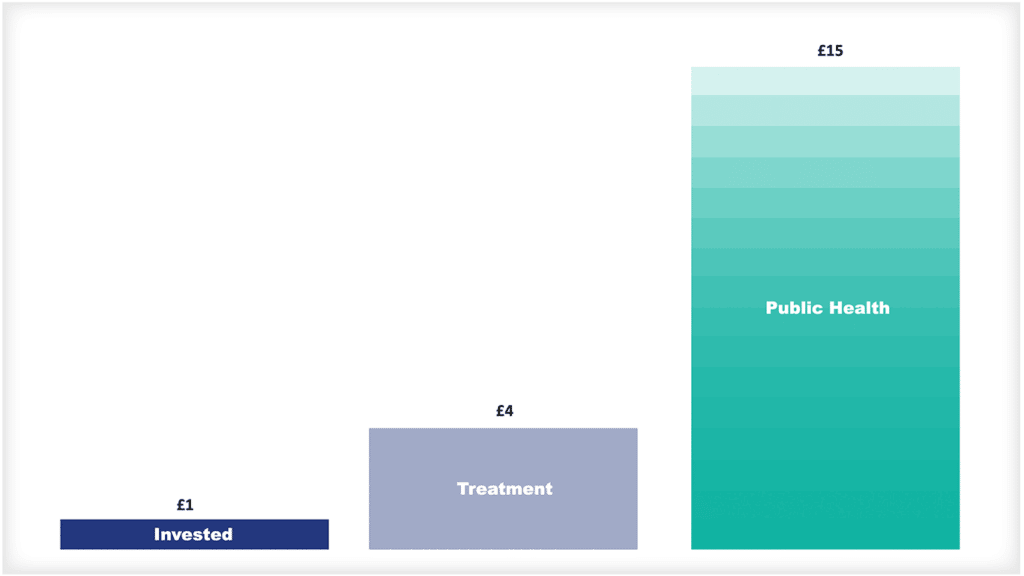
In the same way, when we make decisions about healthcare, we are always weighing the costs and benefits of different options. We want to get the most value for money, from our taxes or our insurance premiums, or even payments we make ourselves for treatment and care.
Economic value is the value that a person places on an economic good based on the benefit they derive from it. Often value is measured by how much a person is willing to pay for it, but is often not that simple, especially within a health system.
The value to a patient is different to a citizen or society, so many factors have to be considered when determining economic value.
Scarcity
Scarcity exists where there is a gap between the availability of a good and potentially unlimited wants. Scarcity creates a situation of opportunity cost, as individuals and businesses make decisions about how to allocate their resources.
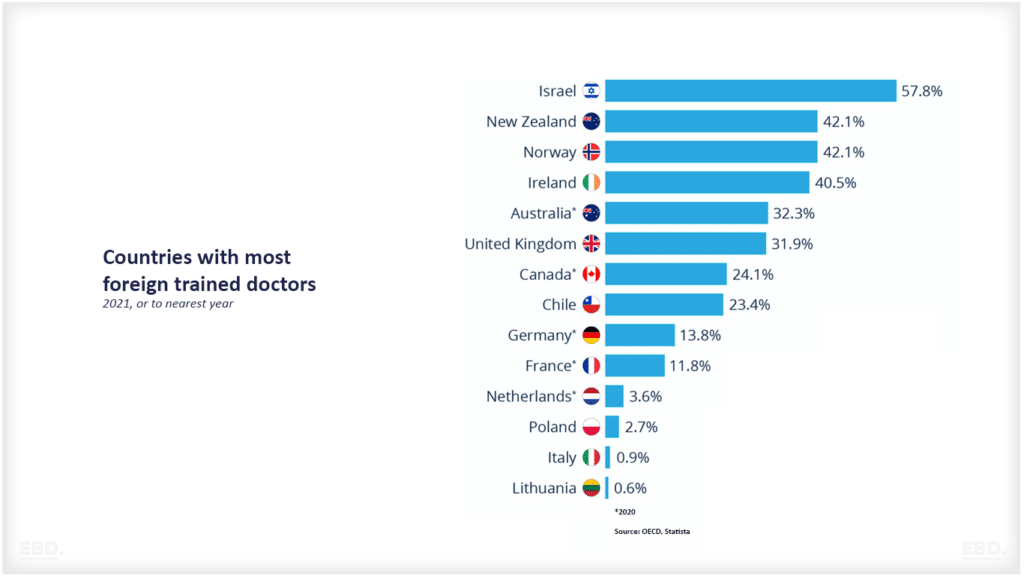
In the healthcare context, scarcity refers to the limited availability of resources such as doctors, hospitals, and medical supplies. This can lead to long waiting times for care, rationing of services, and other problems.
Health economists use the concept of scarcity to understand how the healthcare system allocates resources. They use this understanding to develop policies and recommendations that can improve the efficiency and effectiveness of the healthcare system.
Opportunity Cost
When making choices between scarce goods, the opportunity cost is the value of the next best alternative. In other words, it is the cost of foregone opportunities. This concept is closely related to the concept of scarcity.
In the healthcare context, opportunity cost refers to the value of the health outcomes that are not achieved because of the limited availability of resources. For example, if a patient has to wait a long time for care, they may experience a deterioration in their health status and/or be unable to work. This deterioration in health status is the opportunity cost of waiting for care.
Rationality
People make rational decisions. This means that they weigh the costs and benefits of their options and choose the one that gives them the most value. Of course, in reality, people are not always perfectly rational. We may make decisions based on emotion or misinformation. But in general, this principle holds true.
In the healthcare system, patients and providers often have to make complex decisions with imperfect information. For example, a patient may need to choose between different treatments for a serious illness, without knowing which one will be most effective. Or a provider may need to prescribe a new medication that is very expensive and not covered by insurance, without knowing if it will work better than the cheaper alternatives.
In these cases, people usually do the best they can with the information they have. But it is important to remember that they are not always making perfectly informed rational decisions.
Incentives
People respond to incentives. This means that when the cost of something goes up, people are less likely to do it. Conversely, when the cost goes down, people are more likely to do it. Incentives can be financial, such as a tax deduction, or they can be non-financial, such as a law that requires people to wear seatbelts.
In the healthcare system, there are many different types of incentives that can affect the decisions of patients, providers, and payers. For example, a patient may be more likely to get a preventive check-up if it is free to them. Or a provider may be more likely to prescribe a generic drug compared to a branded drug if it is on the formulary of their patients’ insurance plans, or they are likely to save money by doing so.
Incentives can also be negative, such as when there is a financial penalty for not getting a preventive check-up. In this case, the patient may be more likely to get the check-up because they do not want to pay the penalty.
Markets
Markets are efficient at allocating resources. A market exists where goods and services can be exchanged, typically using a common unit of currency. The demand for a good or service tends to increase as its price falls relative to the opportunity cost. Conversely, the supply of a good or service tends to increase as its relative scarcity increases.
In a free market, prices are determined by the interaction of supply and demand.
Markets work best when there is competition. This means that suppliers have to compete with each other to win customers and there are many customers with choices to make.
Market Failure
There are times when markets do not work well. This is called market failure.
One reason for this is when there is a monopoly. This is when there is only one company that produces a good or service. The company can then charge whatever price they want, without competition to keep prices down.
Another reason for market failure is when there is an externality. This is when the cost or benefit of a good or service is not borne by the people who are consuming it. For example, pollution from a factory may cause health problems for nearby residents. But the factory does not have to pay for these health problems. The residents do. This is an example of a negative externality.
Externalities can be positive as well as negative. For example, if a new hospital is built in a community, it may attract new businesses and jobs to the area. This is an example of a positive externality.
Another reason is that the good is a public good and is available to everyone and cannot be excluded from anyone. A classic example of a public good is clean air. Everyone in the country benefits from it, but it is not possible to exclude anyone from its benefits.
Another reason markets may not work well is when there is an information asymmetry. This is when one party to a transaction has more information than the other. For example, a patient may not know as much about their medical condition as their doctor does. This can lead to problems because, in a pure market situation, the party with more information can take advantage of the other party. For example, a patient may not know if a treatment is necessary or not. The doctor may be able to sell them a treatment that is not helpful.
In a healthcare system, these reasons for market failure feature very strongly. You can’t rely on the market alone to allocate goods and services efficiently and effectively.
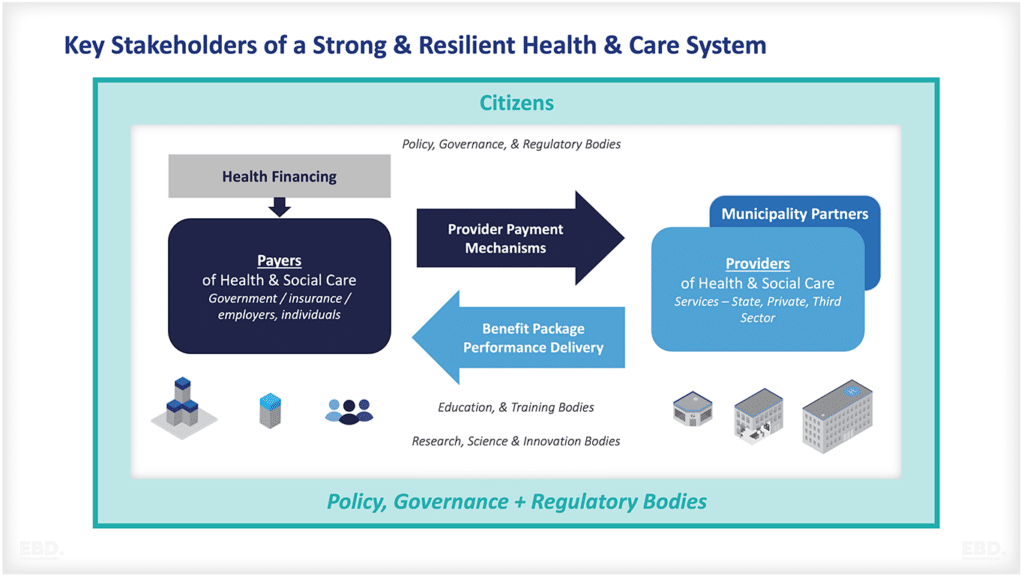
Government
Government has a role to play in ensuring that markets work well. This means that the government should create and enforce rules that protect consumers, promote competition, and ensure that essential services are available to everyone.
In the healthcare system, the government’s role includes funding healthcare directly, managing healthcare delivery directly, managing the healthcare system, and regulating insurance companies, pharmaceutical companies, and non-government providers. The government also provides funding for research and development, and for programs that help to make care more affordable for people who cannot pay for it themselves.
Health economists use the concept of markets and the potential role of government to advise governments on how to manage or regulate the healthcare system to improve the value it creates.
Techniques used by economists
Economists use lots of techniques in their quest to understand and improve value.
Microeconomics
Microeconomics is the study of how individuals and businesses make decisions about how to allocate their resources. It focuses on how these decisions affect the prices of goods and services in the market.
Health economists use microeconomic principles to understand how patients and providers make decisions about healthcare, with a focus on more single actions.
Macroeconomics
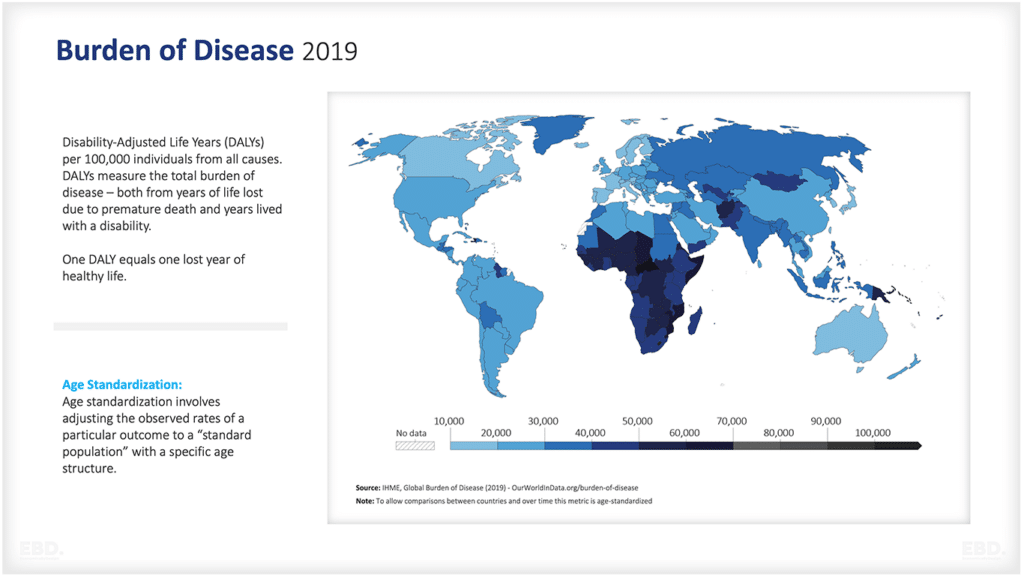
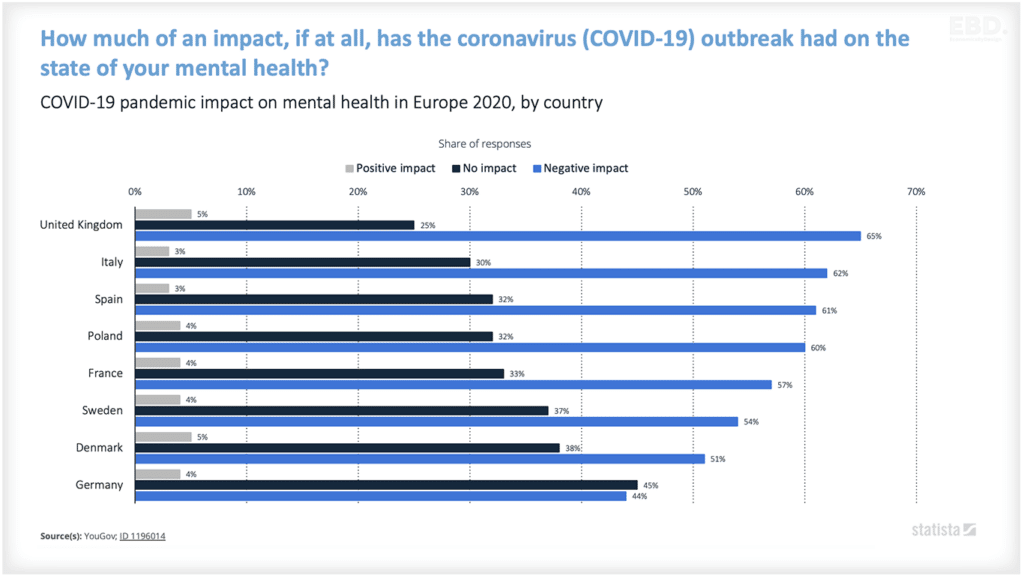
Macroeconomics is the study of how the overall economy works. It focuses on issues such as inflation, unemployment, and economic growth.
Health economists use macroeconomic principles to understand how the healthcare system works and how it impacts the overall economy.
Behavioural Economics
Behavioural economics is the study of how people make decisions. It combines elements of psychology and economics to understand why people make the choices they do.
Health economists use behavioural economic principles to understand how patients and providers make decisions about healthcare, focusing on the human side of the healthcare system.
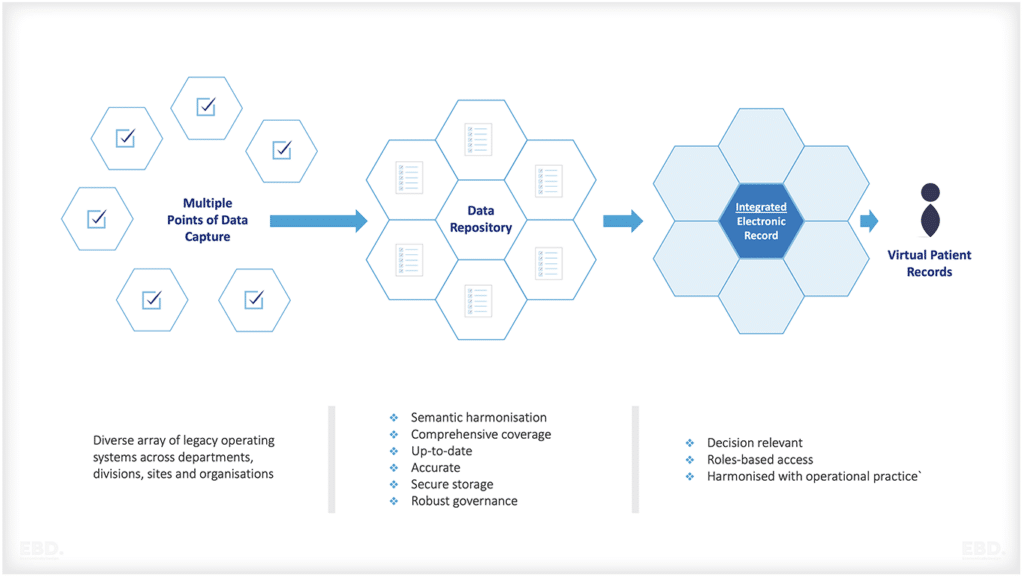
Data Analysis
A large part of health economics is data analysis. Health economists use data to understand how the healthcare system works and to identify areas where it can be improved. They use a variety of statistical techniques to analyze data from sources such as patient surveys, health system performance data, claims data, and data from clinical trials.
Econometrics
Econometrics is a branch of economics that uses statistical methods to analyze economic data. It is often used to test economic theories and to estimate the effect of economic policies.
Health economists use econometric methods to analyze data from sources such as patient surveys, claims data, and clinical trials. They use this analysis to understand how the healthcare system works and to identify areas where it can be improved.
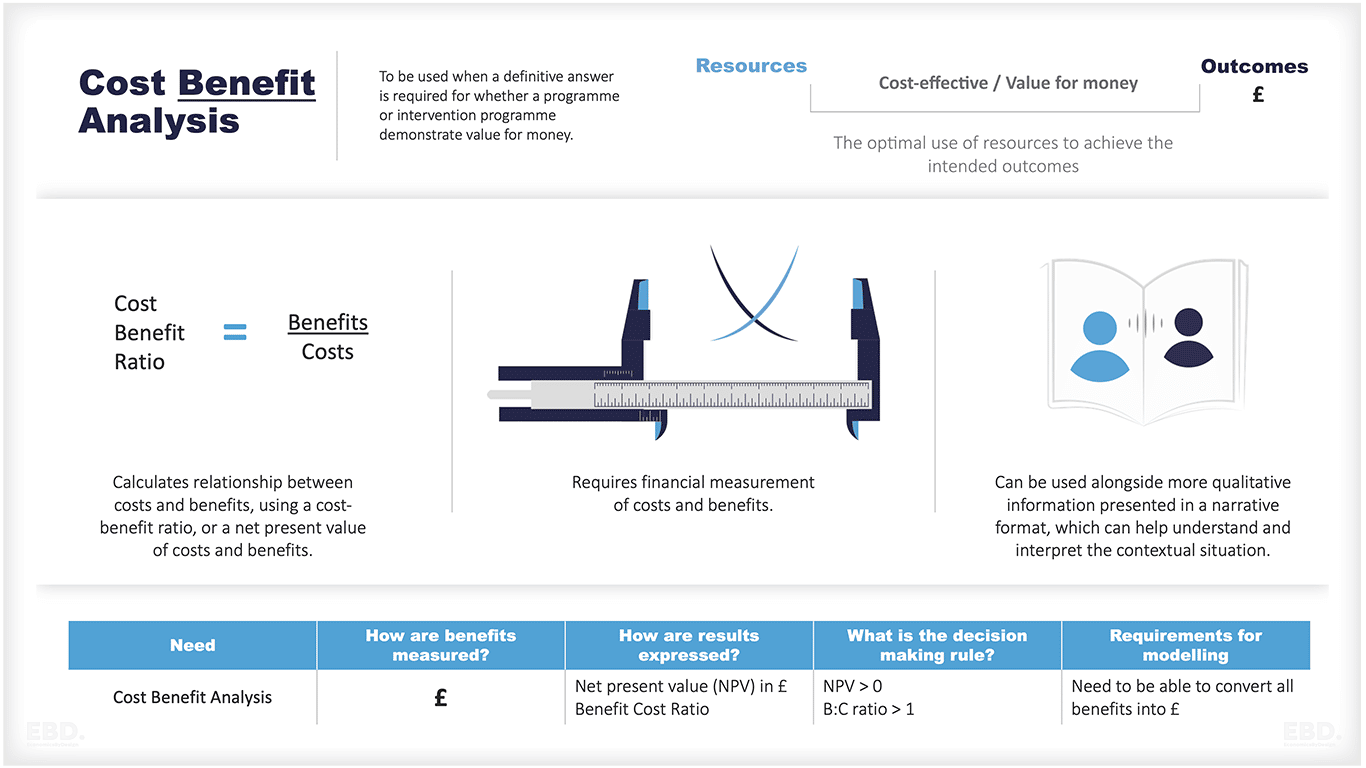
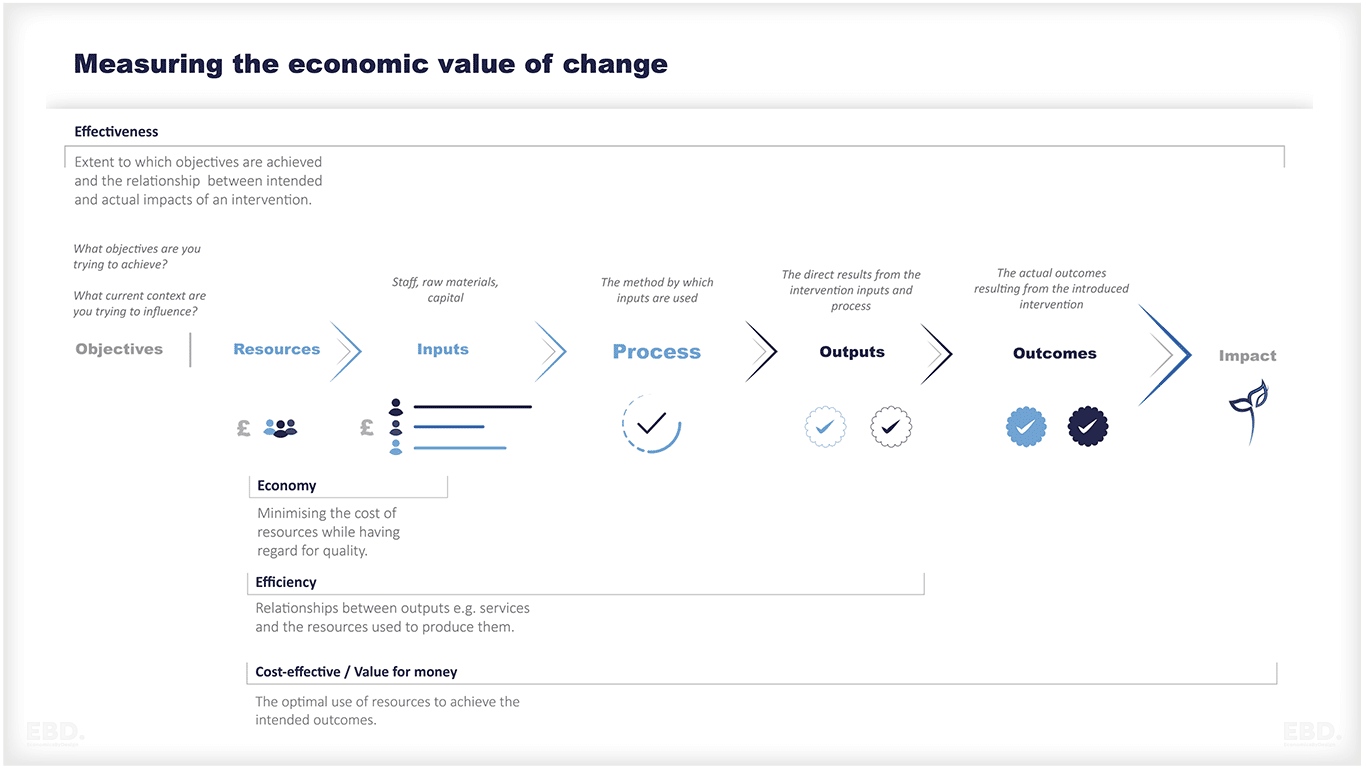
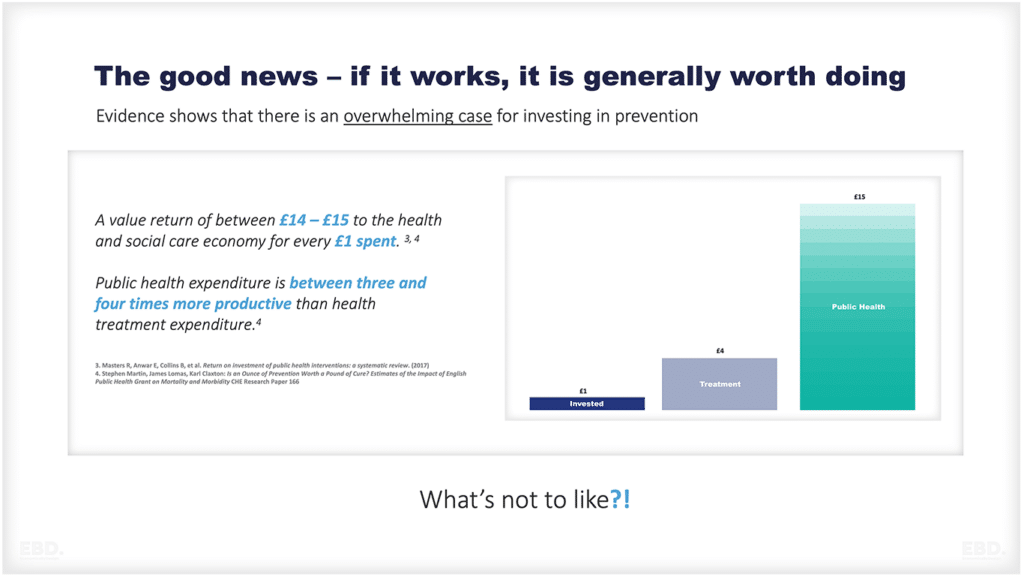
Cost Benefit Analysis
Economists spend a lot of their time helping people to make choices about whether to invest and what to invest in.
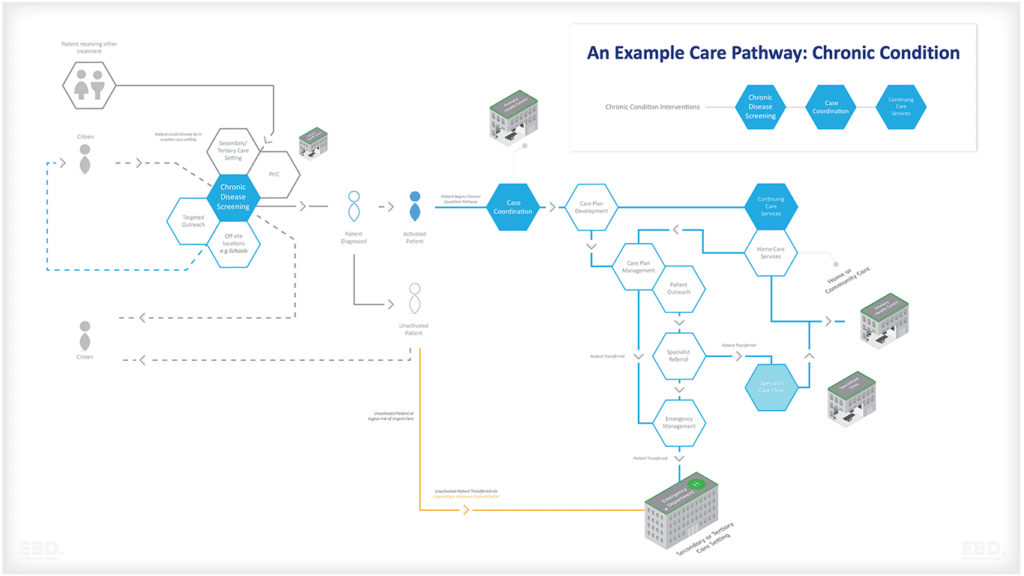
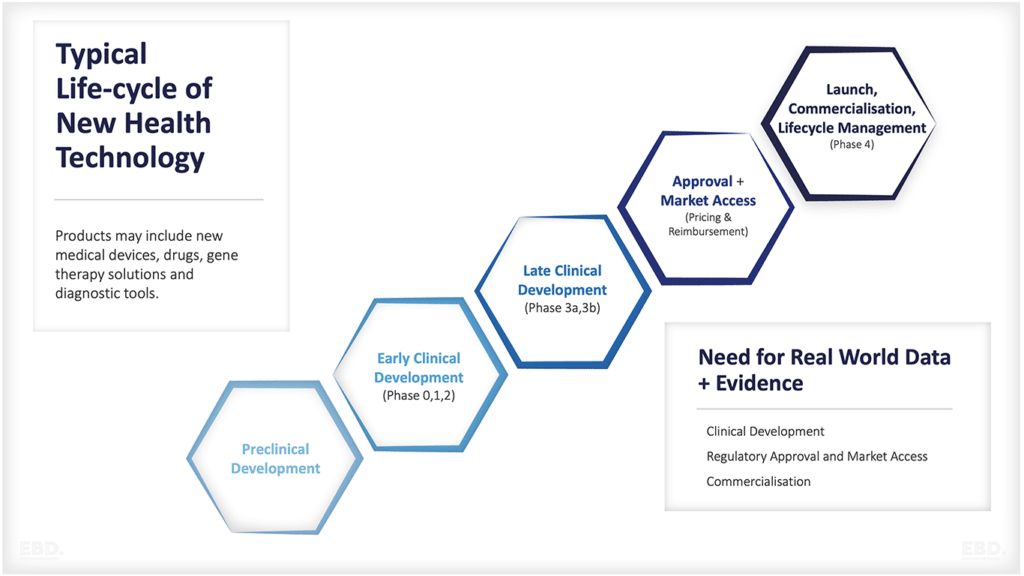
In the health sector this can involve choices about whether and where to build a new hospital, which technology to invest in, which care pathway to develop, or which pharmaceutical product or medical device to procure.
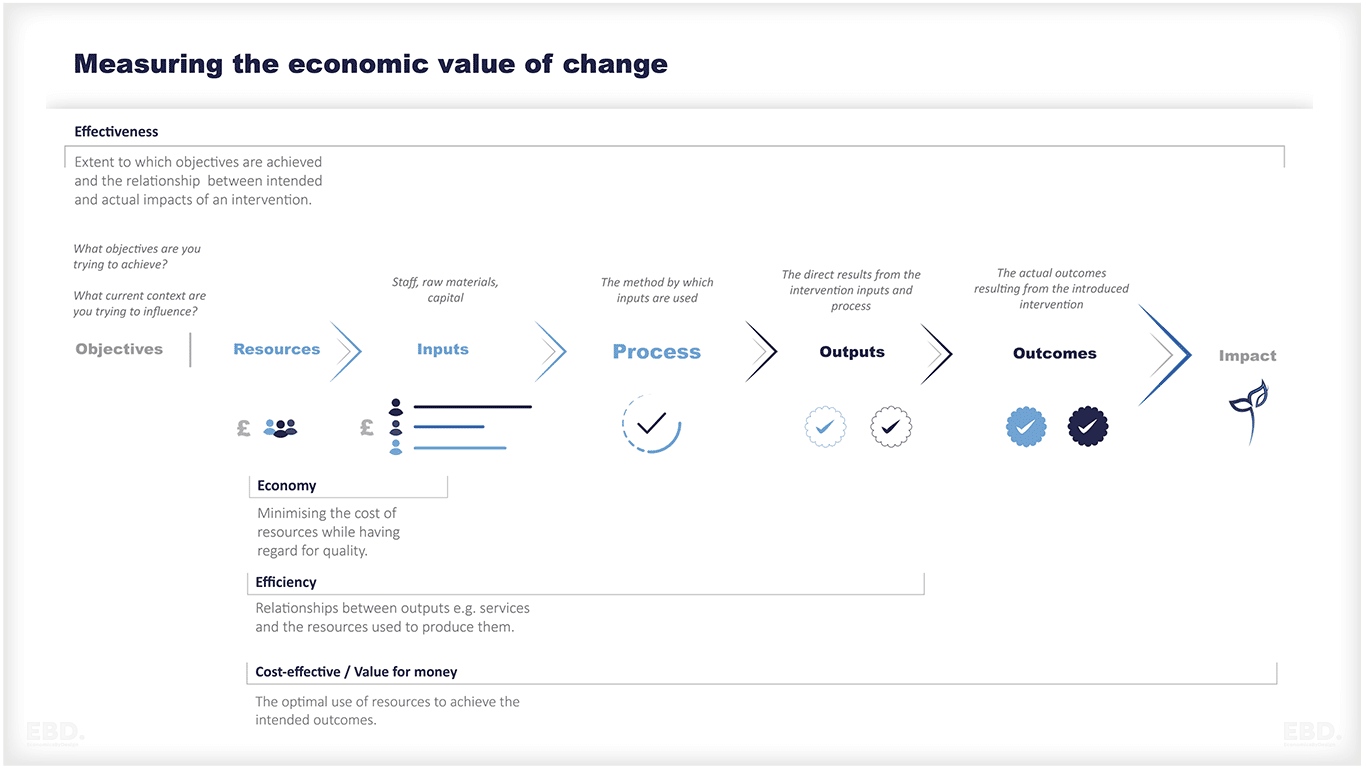
Choices of analysis include:
Cost Economy
Does new intervention involve cheaper input costs than might otherwise be the case, without compromising outcomes?
Cost Efficiency
Does the new intervention deliver a more efficient process than might otherwise be the case, without compromising outcomes?
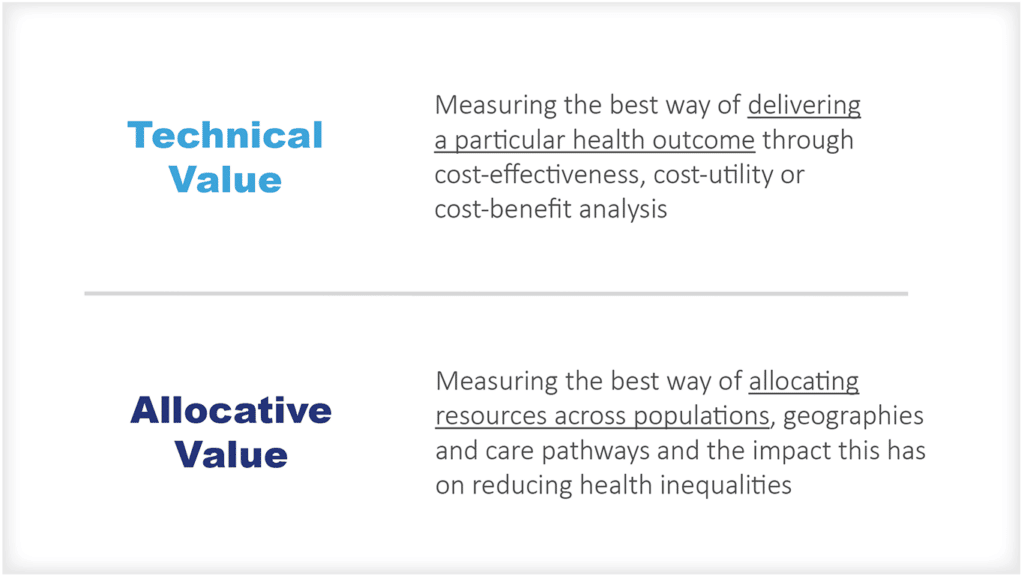
Cost Effectiveness
Does the new intervention require net investment which will be justified by the increased value of outcomes? Where these outcomes can be valued in financial terms, this is known as cost:benefit analysis.
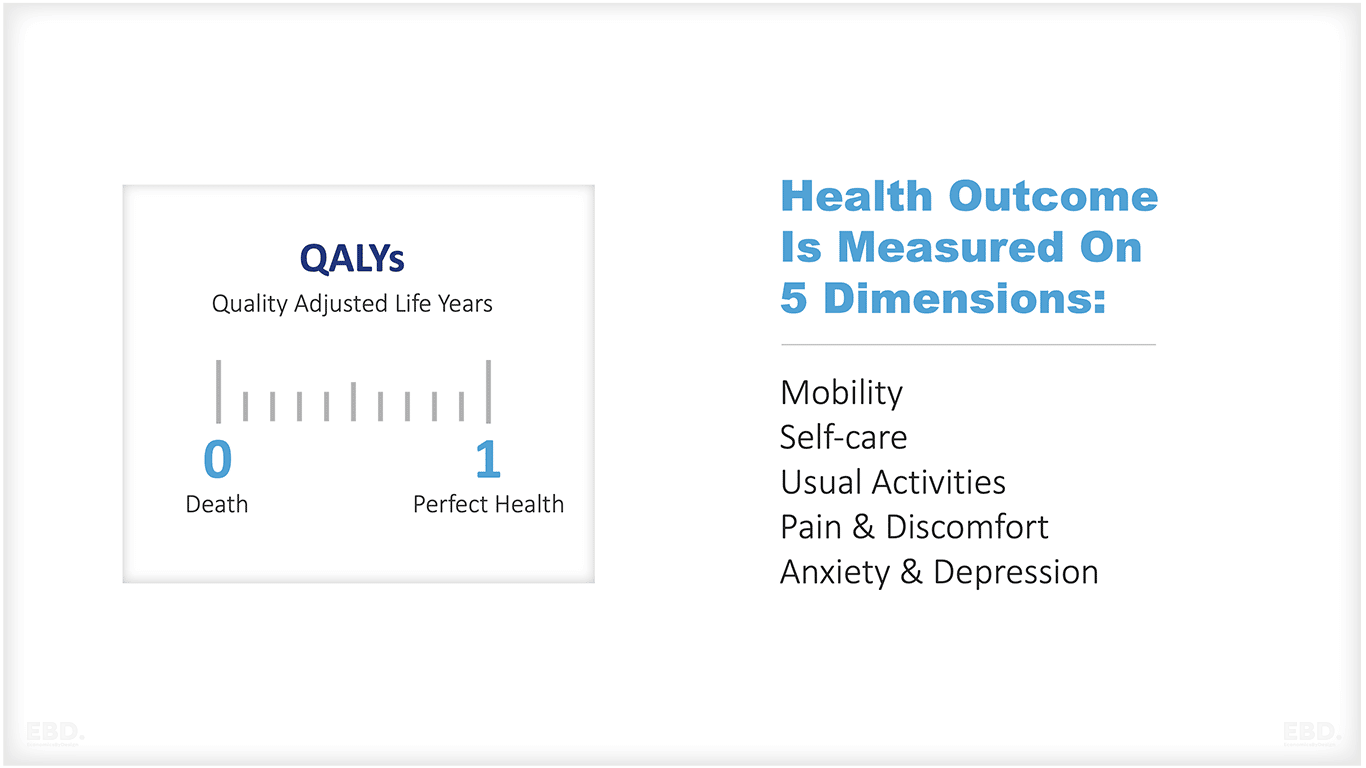
Cost Utility
In healthcare cost-effectiveness analysis often involves cost-utility analysis, where the health outcome is measured by its utility value. The most common method of calculating health utility is the Quality Adjusted Life Year or QALY.
A QALY takes into account both the quantity and quality of life years gained. Quality of life is often measured using a generic instrument such as the EQ-5D which captures 5 dimensions of health – mobility, self-care, usual activities, pain/discomfort, anxiety/depression.
Each dimension can be scored from 1 (no problems) to 3 (severe or extreme problems). A health state can then be described by a specific combination of these dimensions, e.g. 11122. The EQ-5D has a standard set of weights which map these health states onto a scale from 0 (death) to 1 (full health).
The quality of life weights can be used to calculate the QALYs gained from an intervention. The cost per QALY provides a way of comparing different interventions across different patient groups and health conditions.
In the NHS in England, the NICE reference case is that a cost per QALY of £20,000 – £30,000 is considered good value for money relative to other outcomes which could be achieved from health expenditure.
NICE may also recommend an intervention with a cost per QALY of up to £50,000 if it offers particular benefits such as health gains for people with very poor health. The Government estimates that the average societal value of a QALY is £70,000. Please see our other article on the WELLBY.
Challenges in health economics
Health economics is a complex and rapidly evolving field. As such, it faces a number of challenges, including:
- Ensuring the quality of data
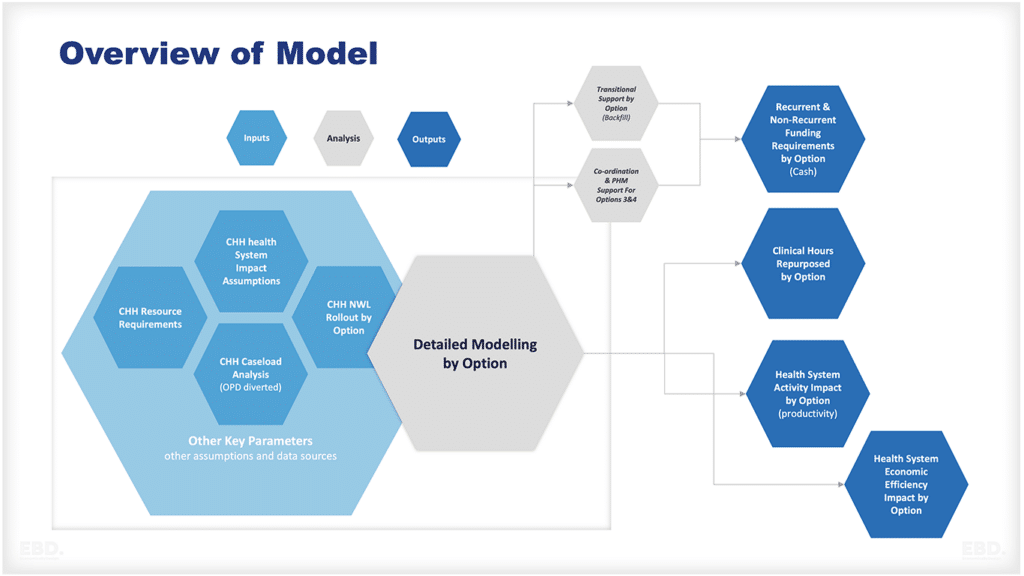
- Managing the complexity of models
- Communicating findings to non-experts
- Dealing with the political nature of some of the issues
- Addressing the ethical implications of some of the work
- Ensuring that research is evidence-based and rigorous
- Managing the expectations of stakeholders
- Building capacity in low-and middle-income countries
- Improving the coordination of research efforts
- Fostering interdisciplinary collaboration
Despite these challenges, health economics is a critical field that can make a valuable contribution to the improvement of health and healthcare around the world.
The future of health economics
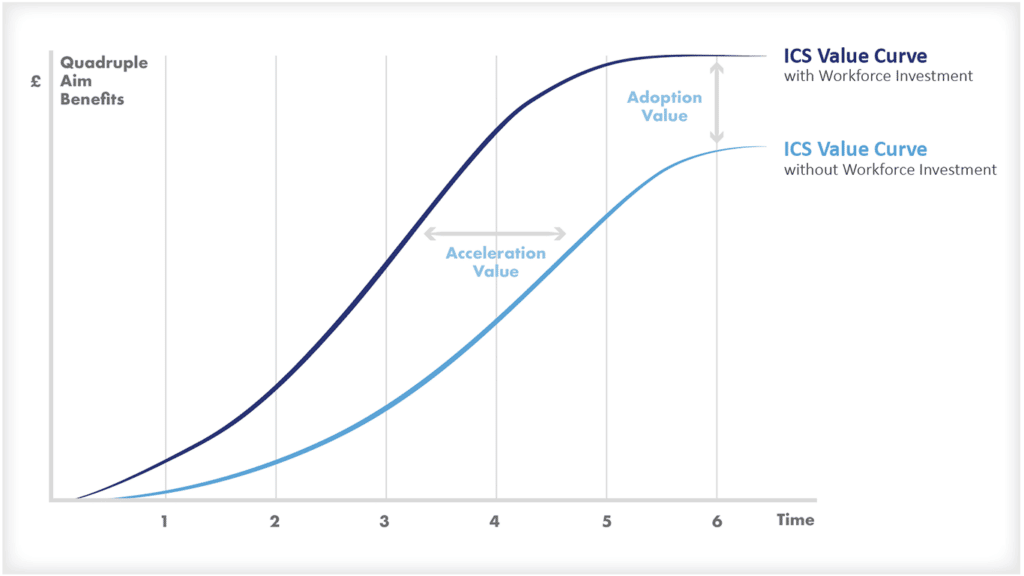
The field of health economics is constantly evolving. As our understanding of the healthcare system improves, so too does our ability to make it more efficient and effective.
Some of the areas that are likely to receive increasing attention in the future include:
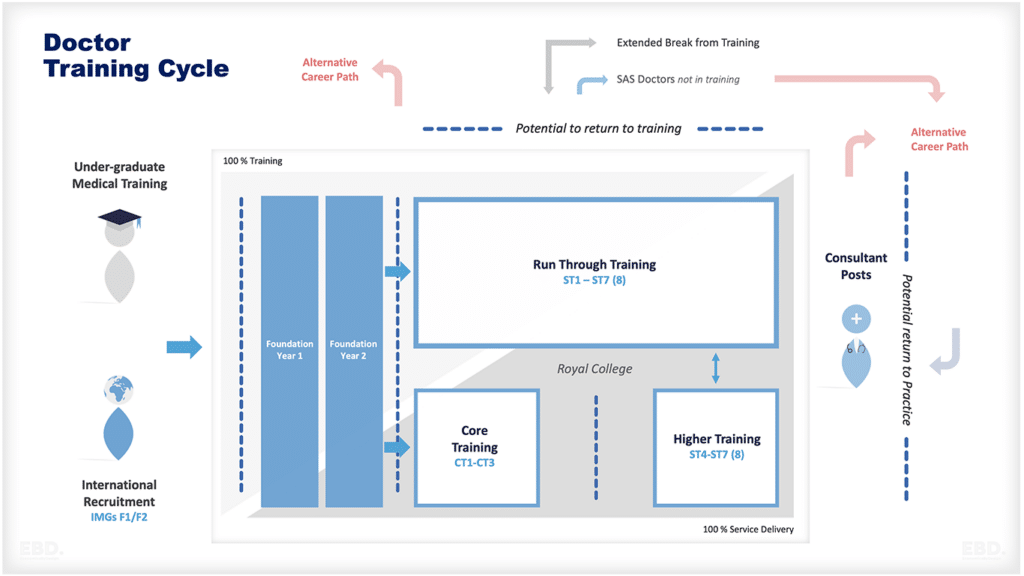
- The impact of technology on the healthcare system
- The role of big data in improving decision-making
- The use of artificial intelligence in healthcare
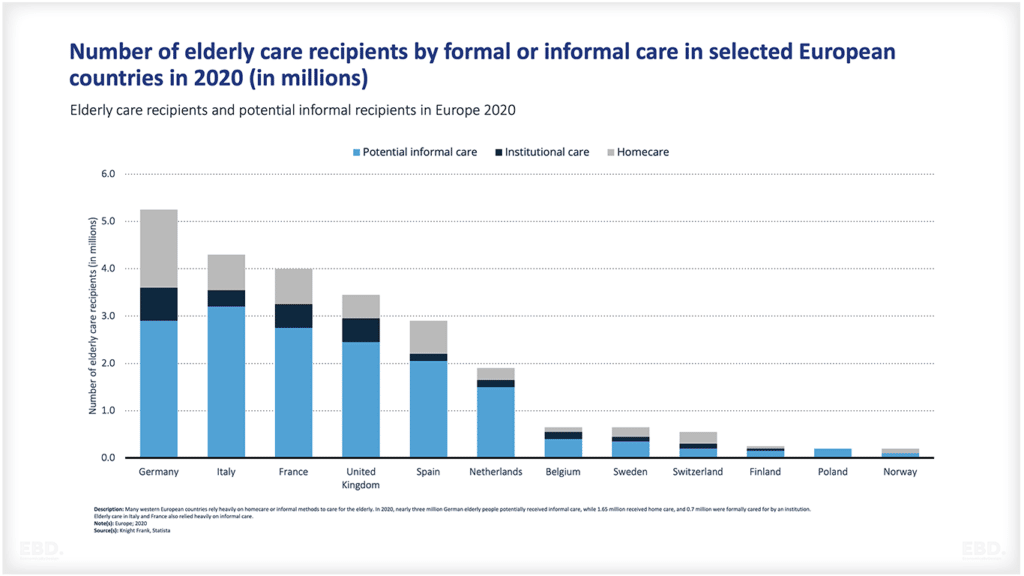
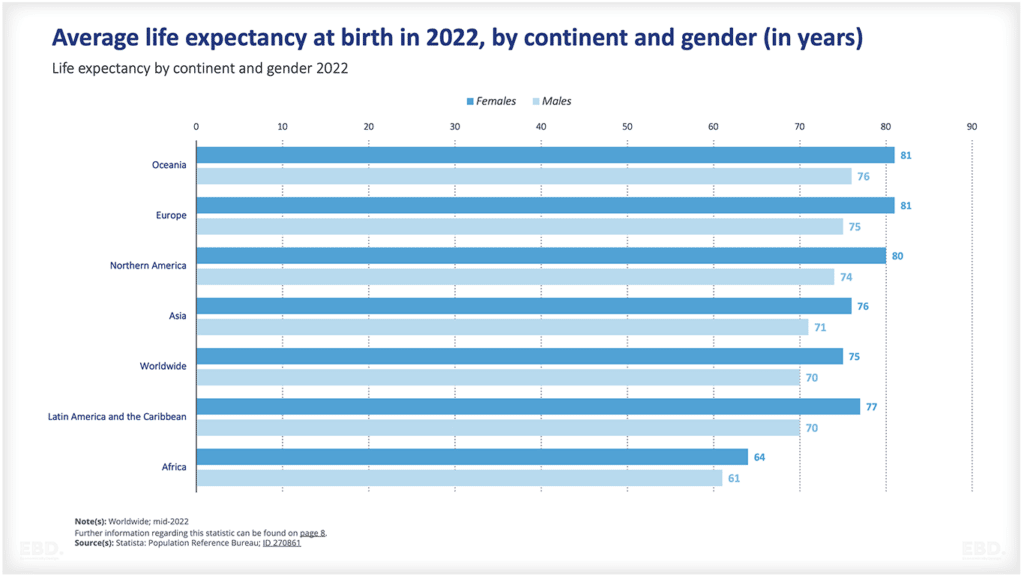
- The opportunities and challenges posed by an ageing population
- The implications of Brexit for the UK healthcare system
How can health economists add value?
Health economists can add value to the healthcare system by improving our understanding of how it works and by making recommendations on how to improve its efficiency and effectiveness.
Health economists play a vital role in the healthcare system, and their work can have a profound impact on the lives of individual patients as well as on the overall effectiveness of the healthcare system.
Health economics is increasingly being used to inform decision-making at all levels of the health system.
Some examples of how it is being used include:
- In the UK, the National Institute for Health and Care Excellence (NICE) uses cost-effectiveness analysis to assess whether new drugs and treatments represent good value for money for the NHS.
- The US Affordable Care Act includes a number of provisions that are based on the principles of health economics, such as the individual mandate, which requires people to have health insurance or face a financial penalty.
- In Australia, the Pharmaceutical Benefits Scheme (PBS) uses cost-effectiveness analysis to assess whether new drugs should be subsidised by the government.
- The World Health Organization (WHO) uses health economics to inform its decision-making on a range of issues, such as which diseases to target with its vaccination programmes or implementing payment models.
- Pharmaceutical companies are using health economic evaluation to help them decide which new drugs to develop and bring to market.
- Health insurers are using health economic principles to design new insurance products and to assess the value of existing ones.
- Medical device companies are using cost-effectiveness analysis to demonstrate the value of new medical technologies.
- Hospitals are using health economic principles to make decisions about which services to offer and how to allocate their resources.
- In India, the government is using health economic principles to guide its decision-making on which new drugs and treatments to make available to the population.
Wherever they work, health economists are helping policy-makers and decision takers to allocate scarce resources to deliver the maximum value in the healthcare sector.
10 ways a health economist can help
If you need help with any of the following, you may want to consider speaking with a health economist:
- Understanding the key concepts in health economics
- Applying health economic principles to real-world problems
- Conducting health economic analysis
- Assessing the value of new drugs and treatments
- Designing new insurance products
- Developing innovative financing mechanisms for healthcare
- Evaluating the impact of government policies on the healthcare system
- Understanding the factors that influence health outcomes
- Modelling the impact of proposed changes to the healthcare system
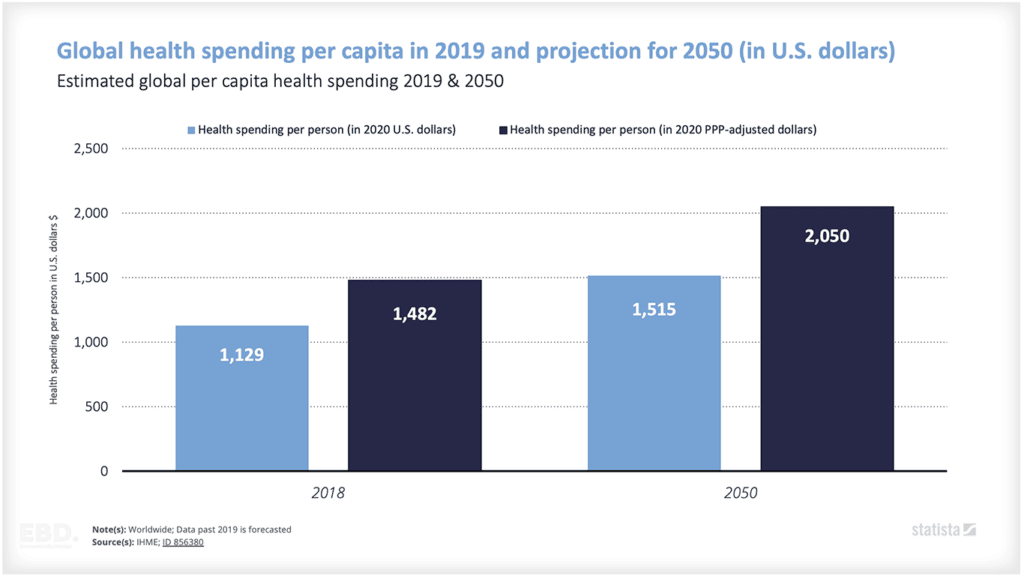
- Forecasting future trends in healthcare spending.
There are many different ways in which health economics can be applied, and it is an increasingly important tool for policy-makers, clinicians and innovators around the world.
If you think that health economics could help you to solve a particular problem, then please don’t hesitate to get in touch.
Amazing